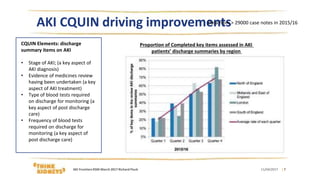
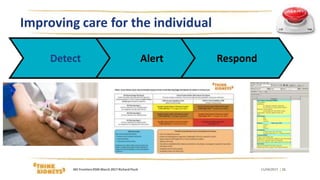
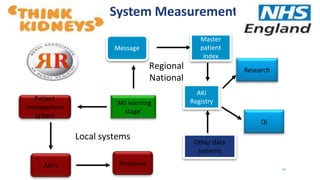
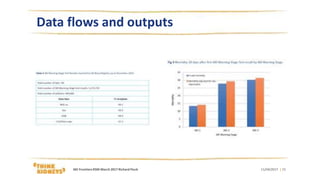
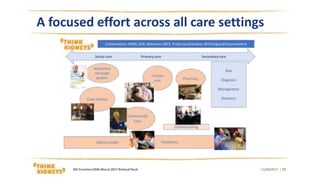
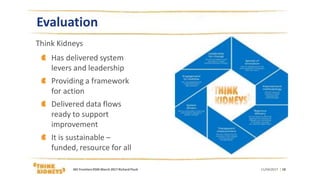
The document evaluates the Think Kidneys program aimed at improving care for acute kidney injury (AKI) through collaboration, education, and quality improvement. It highlights the need for clear data flows, clinicians' education, and key elements like discharge summaries to enhance patient safety. The program has established a framework for action that promotes systemic improvements in AKI management across various healthcare settings.