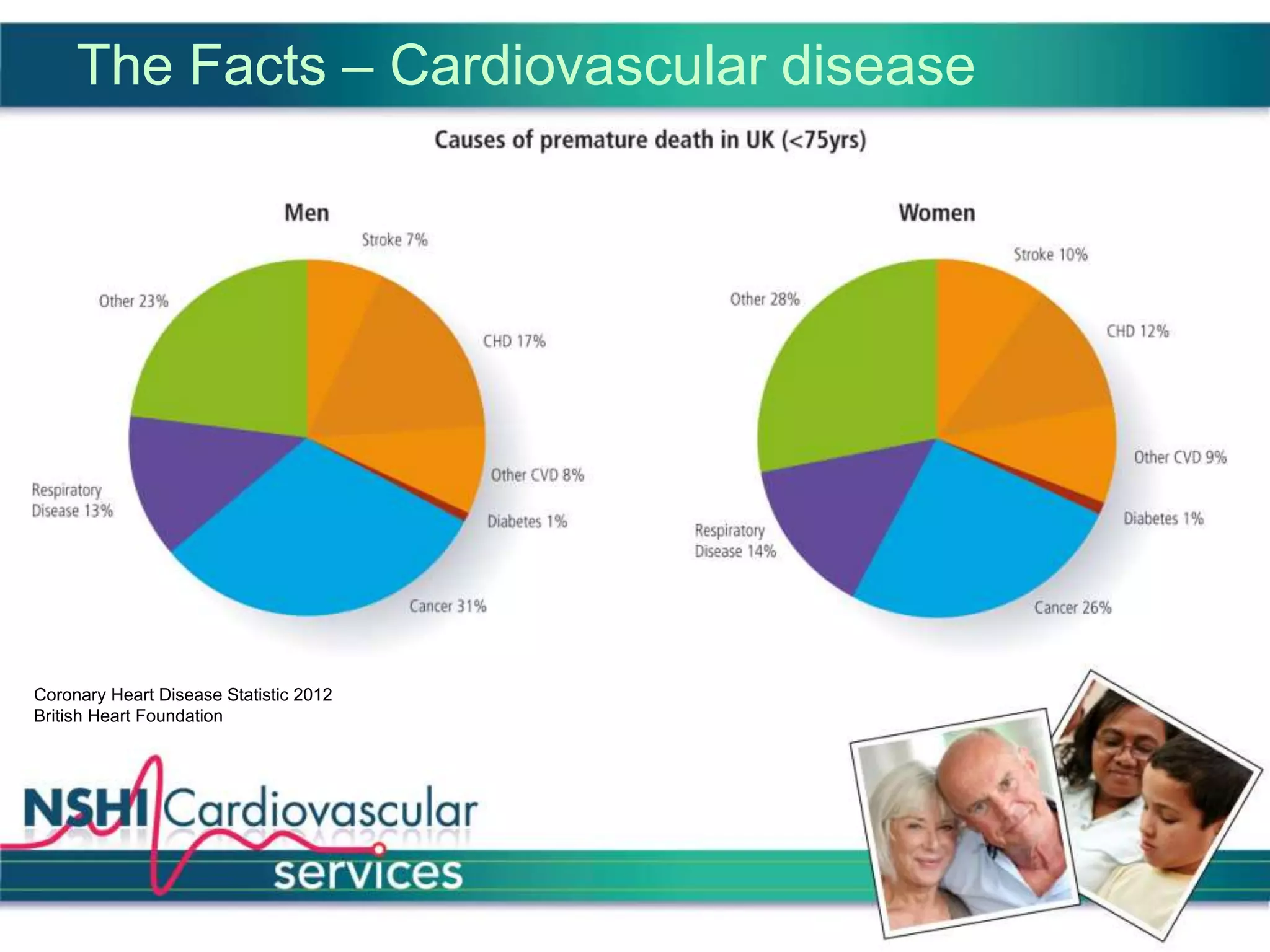
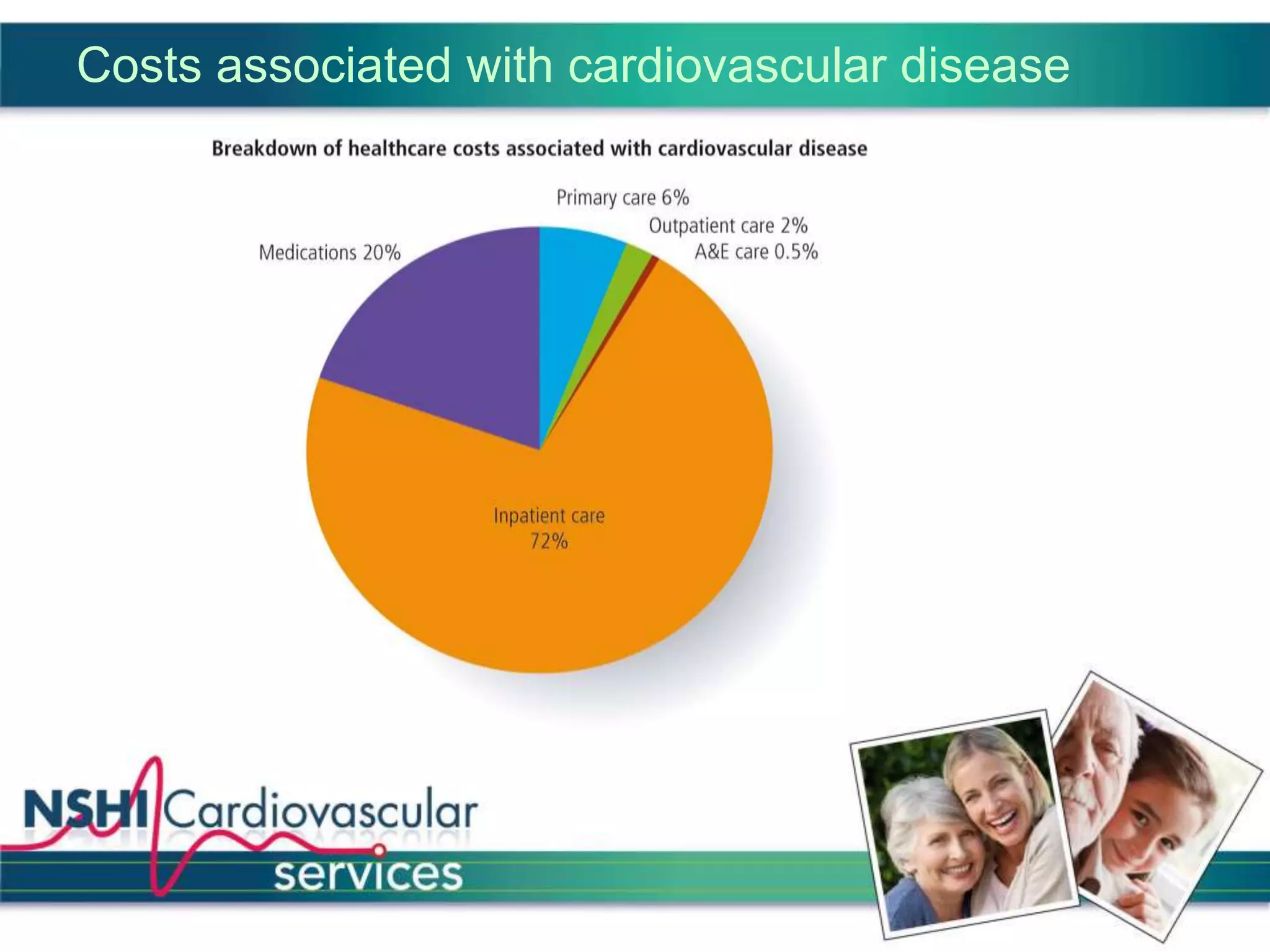
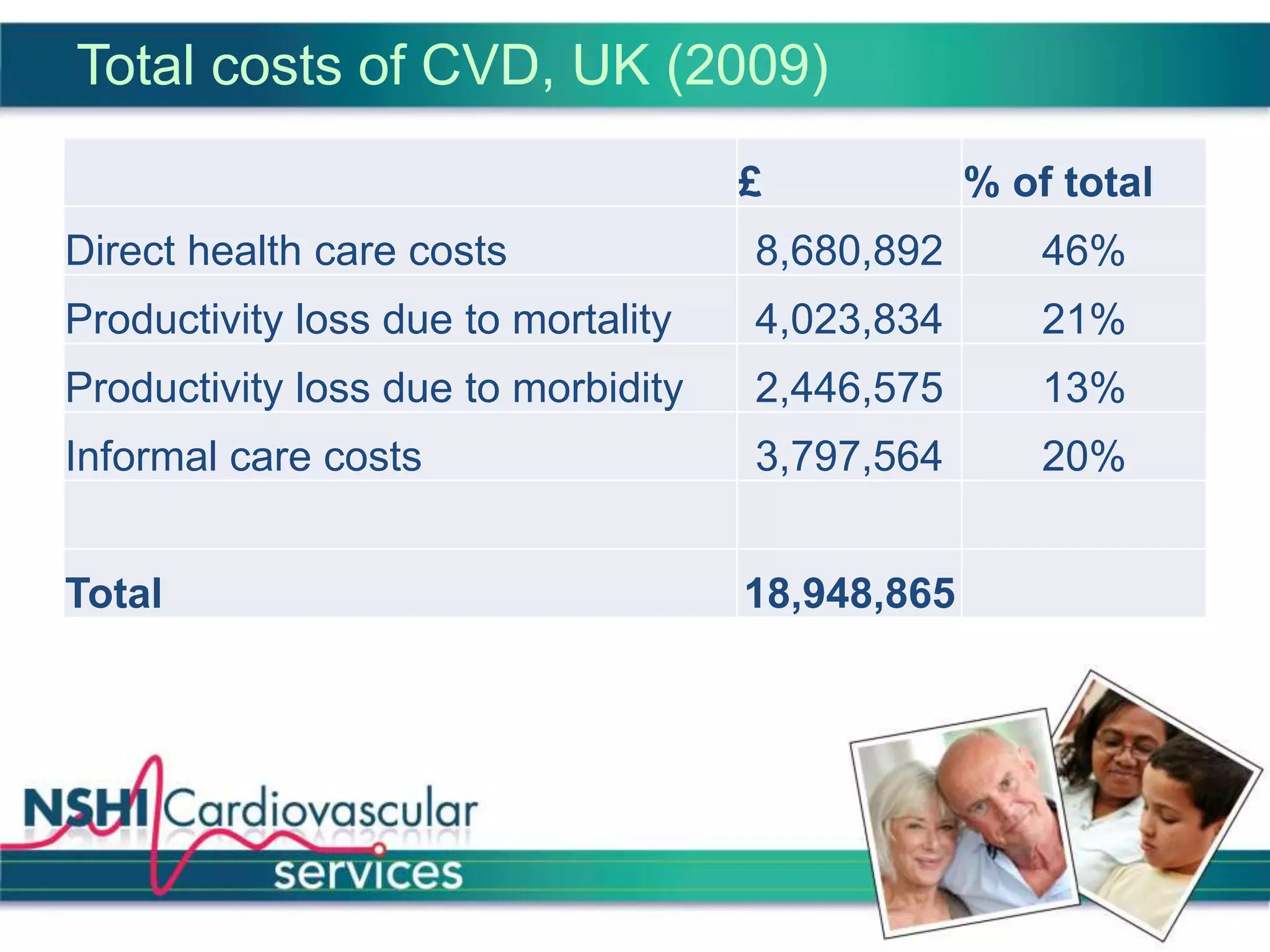
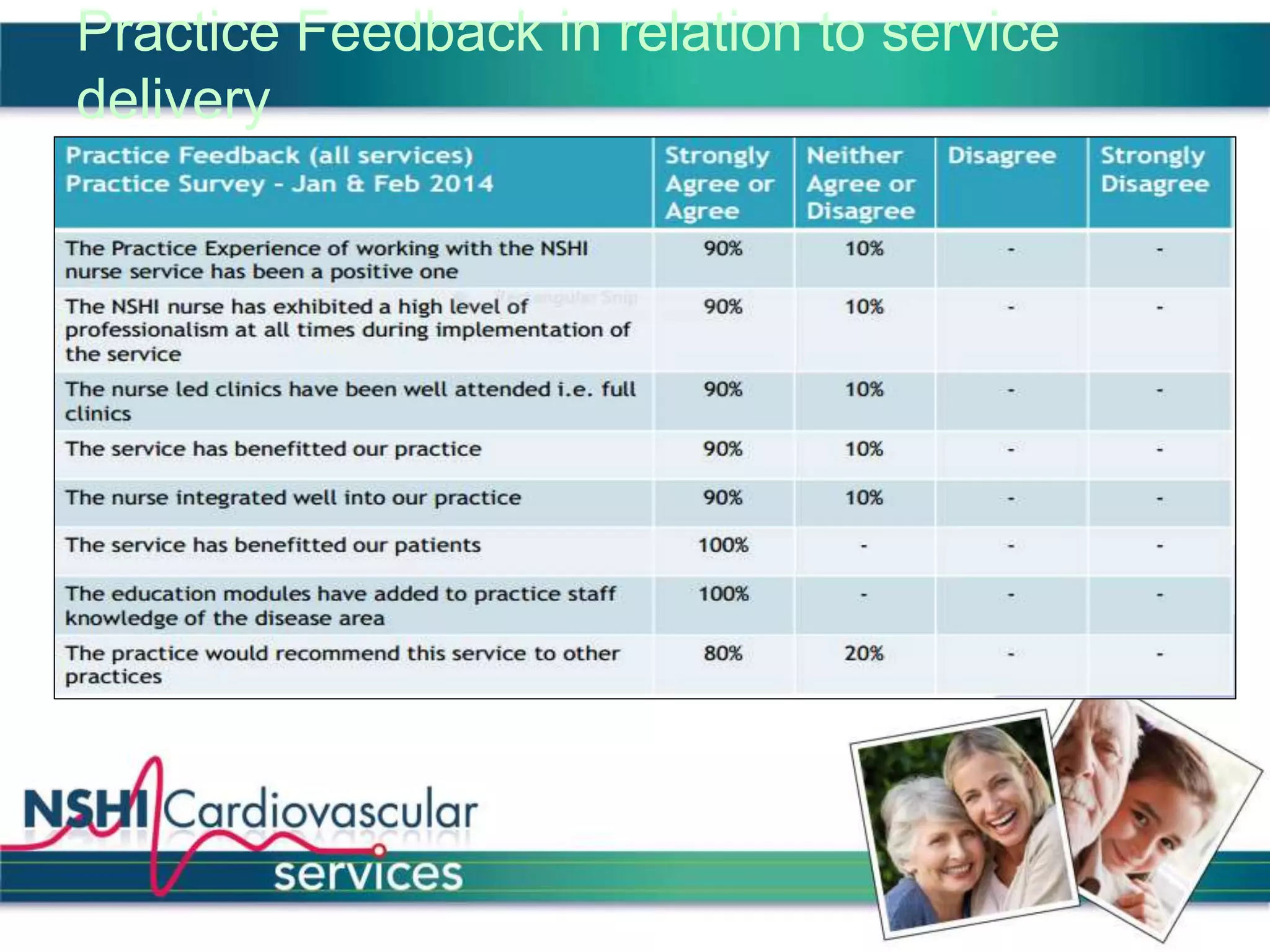
The National Services for Health Improvement (NSHI) cardiovascular programme seeks to address the management and prevention of cardiovascular disease (CVD) in the UK, which accounts for a significant number of deaths and presents varying service quality across regions. The program's goals include improving identification and management of CVD, enhancing patient care, and reducing hospital admissions through integrated services, particularly within primary care. NSHI emphasizes a collaborative approach to meet national guidelines and improve health outcomes for those living with or at risk of CVD.