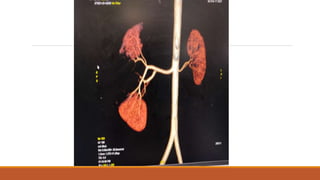
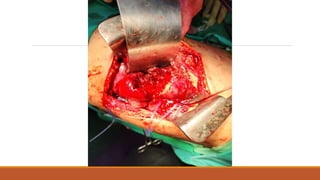
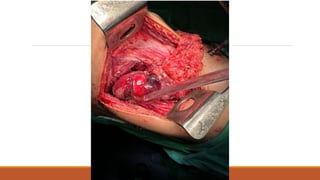
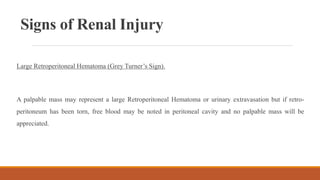
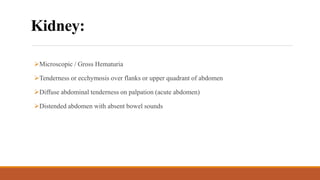
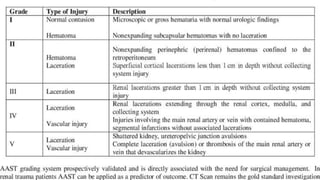
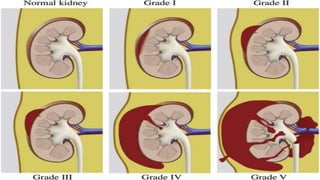
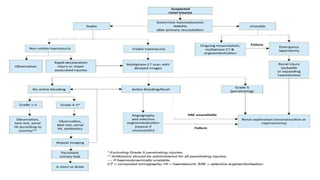
A 14-year-old boy presented to the ER after an RTA with abdominal distension and tenderness, vomiting, and hematuria. Imaging showed a subcapsular renal hematoma of 150-200ml. The mechanism was blunt trauma from the RTA. Based on imaging findings, it is a Grade 3 renal injury. Evaluation includes hemodynamic stability, history, and testing for hematuria. Management is usually non-operative for Grade 1-4 injuries, with angioembolization for bleeding. Options include exploration for hemodynamic instability or high grade injuries.