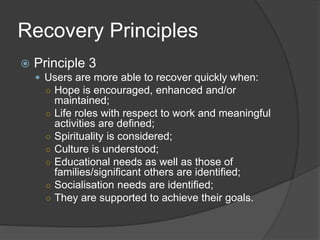
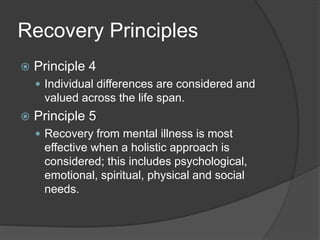
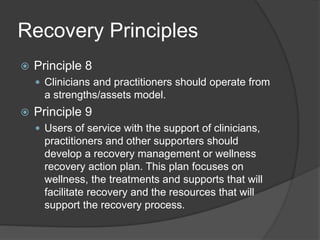
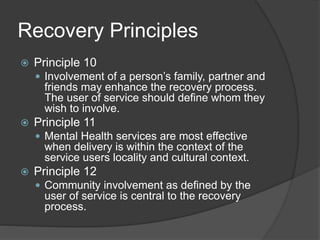
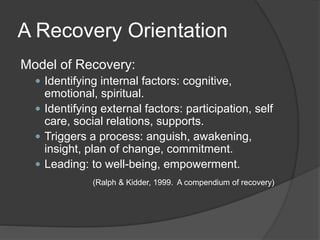
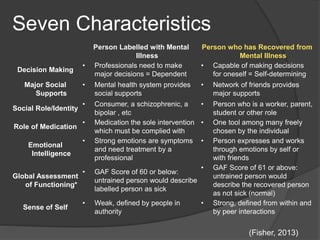
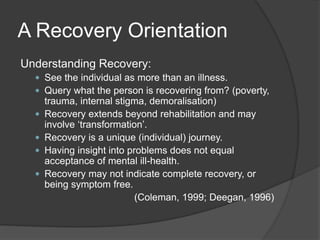
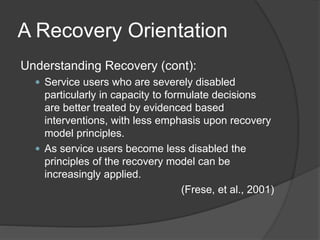
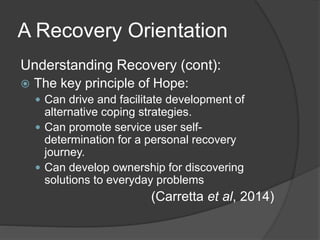
The document discusses various concepts and principles related to recovery from mental illness. It provides multiple definitions and perspectives on what recovery means, including that it is a personal process rather than simply an end to symptoms. Recovery involves maximizing quality of life and taking responsibility for one's life within limitations caused by mental illness. The document also outlines 12 principles of a recovery-oriented approach, such as emphasizing hope, functioning from a strengths-based perspective, and involving social supports.