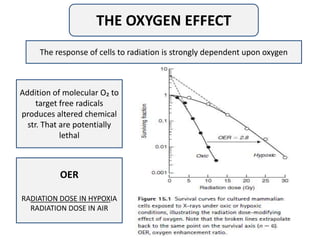
This document discusses radiation response modifiers in cancer treatment, emphasizing the relationship between radiation dose, tumor response, and normal tissue damage. It highlights strategies to enhance therapeutic efficacy, such as hypoxic cell sensitizers, novel chemotherapy agents, and concurrent chemoradiation approaches while addressing challenges like treatment toxicity and anemia. The document also mentions the evolving role of radioprotectors and advanced treatment methods, noting that while some preclinical candidates show promise, their success in phase III trials has been mixed.