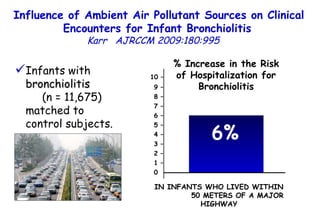
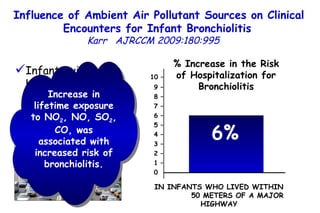
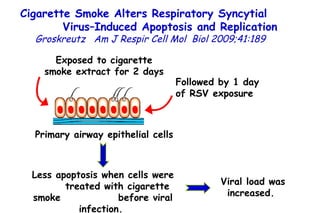
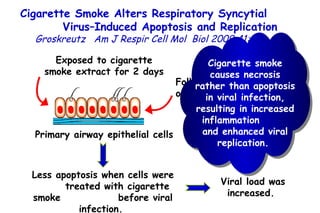
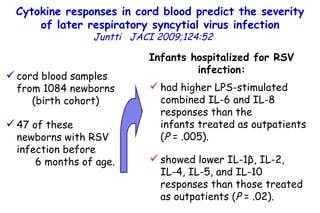
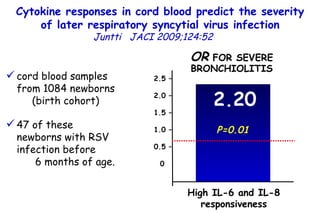
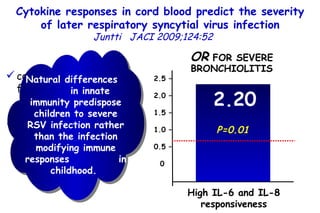
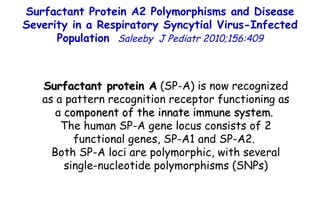
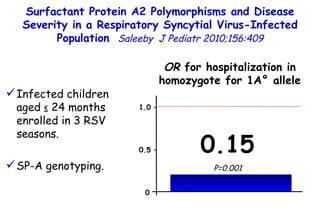
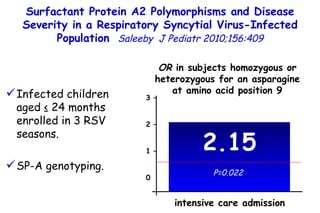
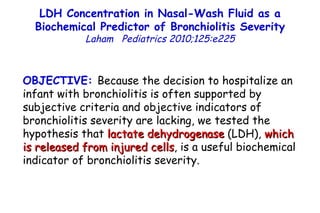
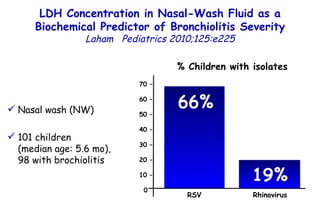
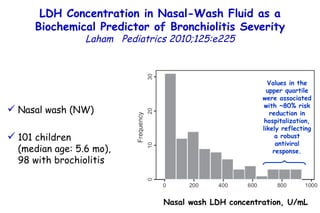
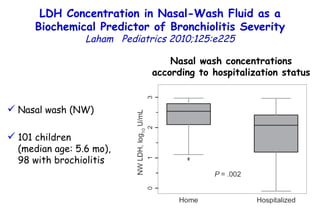
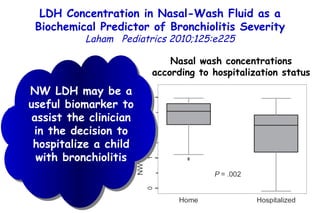
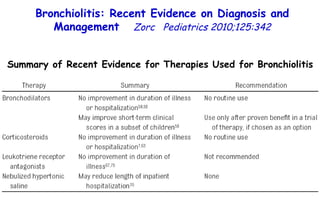
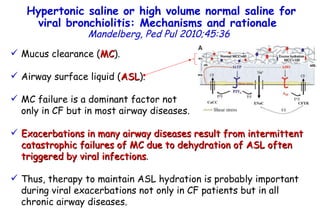
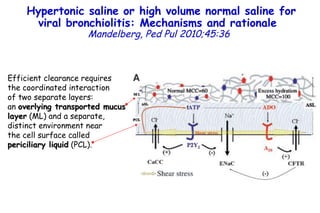
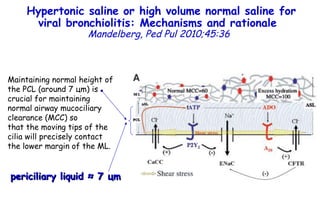
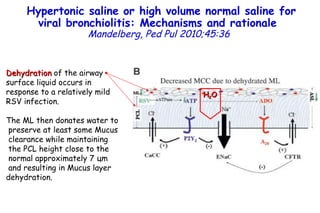
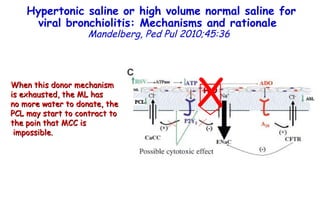
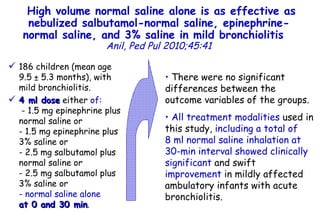
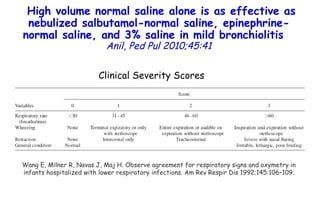
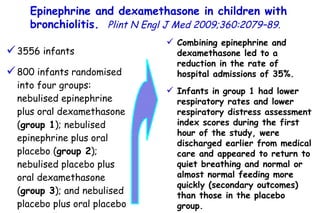
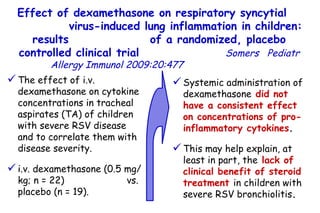
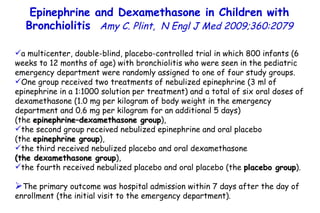
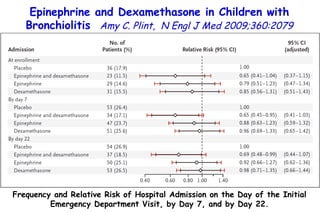
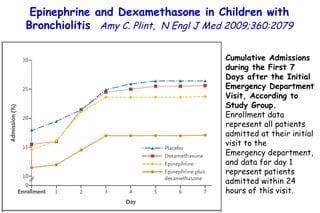
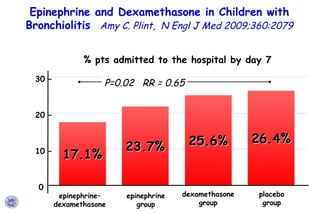
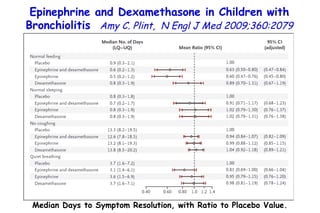
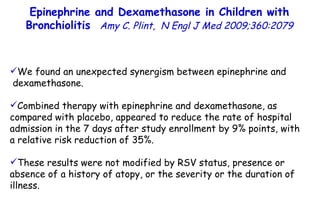
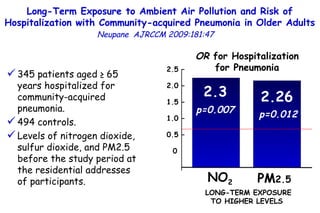
The document discusses several studies on bronchiolitis. It finds that living near a major highway is associated with a 6% increased risk of hospitalization for bronchiolitis. Cigarette smoke exposure decreases apoptosis and increases viral load during RSV infection. High cord blood levels of IL-6 and IL-8 are associated with more severe bronchiolitis. Certain surfactant protein polymorphisms are also linked to increased disease severity and hospitalization risk. A recent study suggests nasal wash lactate dehydrogenase levels may help predict bronchiolitis severity and hospitalization need. Several treatments for bronchiolitis, including hypertonic saline, high-volume normal saline, and nebulized epinephrine or salbut




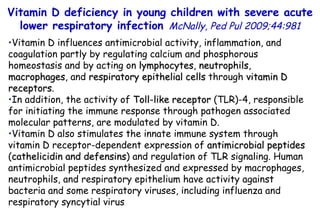
![Serum 25 hydroxyvitamin D [25(OH)D] levels. Young children with bronchiolitis (n = 55) or pneumonia (n = 50). (ALRI) Subjects without respiratory symptoms (n = 92). Vitamin D deficiency in young children with severe acute lower respiratory infection McNally, Ped Pul 2009;44:981](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-90-320.jpg)
![Vitamin D deficiency in young children with severe acute lower respiratory infection McNally, Ped Pul 2009;44:981 Serum 25 hydroxyvitamin D [25(OH)D] levels. Young children with bronchiolitis (n = 55) or pneumonia (n = 50). (ALRI) Subjects without respiratory symptoms (n = 92). The mean vitamin D level for the entire ALRI group was not significantly different from the control group (81 ± 40 vs. 83 ± 30 nmol/L, respectively).](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-91-320.jpg)
![Vitamin D deficiency in young children with severe acute lower respiratory infection McNally, Ped Pul 2009;44:981 Serum 25 hydroxyvitamin D [25(OH)D] levels. Young children with bronchiolitis (n = 55) or pneumonia (n = 50). (ALRI) Subjects without respiratory symptoms (n = 92). 87 49 P=0.001](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-92-320.jpg)
![Vitamin D deficiency in young children with severe acute lower respiratory infection McNally, Ped Pul 2009;44:981 Serum 25 hydroxyvitamin D [25(OH)D] levels. Young children with bronchiolitis (n = 55) or pneumonia (n = 50). (ALRI) Subjects without respiratory symptoms (n = 92). The mean vitamin D level for the ALRI subjects admitted to the pediatric intensive care unit (49 ± 24 nmol/L) was significantly lower (p=0.001) than that observed for both control (83 ± 30 nmol/L) and ALRI subjects admitted to the general pediatrics ward (87 ± 39 nmol/L). P=0.001 87 49](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-93-320.jpg)
![Vitamin D deficiency in young children with severe acute lower respiratory infection McNally, Ped Pul 2009;44:981 Serum 25 hydroxyvitamin D [25(OH)D] levels. Young children with bronchiolitis (n = 55) or pneumonia (n = 50). (ALRI) Subjects without respiratory symptoms (n = 92). P=0.001 Vitamin D deficiency (<50 nmol/L) remained associated with ALRI requiring admission to pediatric intensive care unit after the inclusion of prematurity into a multivariate logistic regression model. 87 49](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-94-320.jpg)



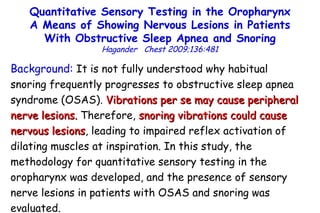
![Quantitative Sensory Testing in the Oropharynx A Means of Showing Nervous Lesions in Patients With Obstructive Sleep Apnea and Snoring Hagander Chest 2009;136:481 Vibration detection thresholds (VDTs) and/or cold detection thresholds (CDTs) were tested at the tonsillar pillars, tongue, lip, and finger. 23 nonsnoring individuals, 13 habitual snorers (apnea-hypopnea index [AHI] < 10), and 31 patients with OSAS (AHI > 20). The tool used for VDT testing with a custom-made intraoral probe. (Vibrameter Type IV; Somedic Inc; Sollentuna, Sweden)](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-451-320.jpg)
![Quantitative Sensory Testing in the Oropharynx A Means of Showing Nervous Lesions in Patients With Obstructive Sleep Apnea and Snoring Hagander Chest 2009;136:481 Vibration detection thresholds (VDTs) and/or cold detection thresholds (CDTs) were tested at the tonsillar pillars, tongue, lip, and finger. 23 nonsnoring individuals, 13 habitual snorers (apnea-hypopnea index [AHI] < 10), and 31 patients with OSAS (AHI > 20). The intraoral probe for CDT testing , using a thermal sensory analyzer. (Medoc 2000 TSA; Medoc Inc; Ramat Yishai, Israel)](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-452-320.jpg)
![Quantitative Sensory Testing in the Oropharynx A Means of Showing Nervous Lesions in Patients With Obstructive Sleep Apnea and Snoring Hagander Chest 2009;136:481 Vibration detection thresholds (VDTs) and/or cold detection thresholds (CDTs) were tested at the tonsillar pillars, tongue, lip, and finger. 23 nonsnoring individuals, 13 habitual snorers (apnea-hypopnea index [AHI] < 10), and 31 patients with OSAS (AHI > 20).](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-453-320.jpg)
![Quantitative Sensory Testing in the Oropharynx A Means of Showing Nervous Lesions in Patients With Obstructive Sleep Apnea and Snoring Hagander Chest 2009;136:481 Vibration detection thresholds (VDTs) and/or cold detection thresholds (CDTs) were tested at the tonsillar pillars, tongue, lip, and finger. 23 nonsnoring individuals, 13 habitual snorers (apnea-hypopnea index [AHI] < 10), and 31 patients with OSAS (AHI > 20).](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-454-320.jpg)
![Quantitative Sensory Testing in the Oropharynx A Means of Showing Nervous Lesions in Patients With Obstructive Sleep Apnea and Snoring Hagander Chest 2009;136:481 Vibration detection thresholds (VDTs) and/or cold detection thresholds (CDTs) were tested at the tonsillar pillars, tongue, lip, and finger. 23 nonsnoring individuals, 13 habitual snorers (apnea-hypopnea index [AHI] < 10), and 31 patients with OSAS (AHI > 20). Signs of sensory nervous lesions were present in the oropharynx of most patients with OSAS and some snorers, supporting the hypothesis of a progressive oropharyngeal nervous lesion.](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-455-320.jpg)
![Determinants of Hypercapnia in Obese Patients With Obstructive Sleep Apnea Kaw Chest 2009;136:787 daytime hypercapnia (PaCO 2 , ≥45 mm Hg) in obese patients (body mass index [BMI], ≥ 30 kg/m 2 ) with OSA (apnea-hypopnea index [AHI], ≥ 5) Metaanalysis of 15 studies (n=4,250) % patients with daytime hypercapnia 19% 20 – 15 – 10 – 5 – 0](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-480-320.jpg)
![Determinants of Hypercapnia in Obese Patients With Obstructive Sleep Apnea Kaw Chest 2009;136:787 daytime hypercapnia (PaCO 2 , ≥45 mm Hg) in obese patients (body mass index [BMI], ≥ 30 kg/m 2 ) with OSA (apnea-hypopnea index [AHI], ≥ 5) 15 studies (n=4,250) % patients with daytime hypercapnia 19% 20 – 15 – 10 – 5 – 0 Patients with hypercapnia had higher BMI (MD, 3.1 kg/m 2 ) and AHI (MD, 12.5) than eucapnic patients.](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-481-320.jpg)
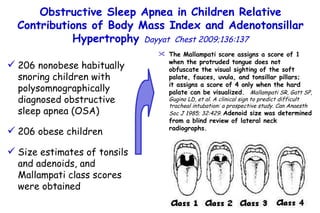
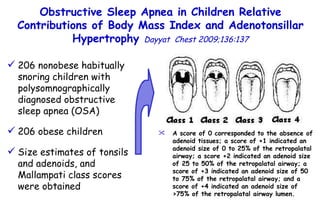
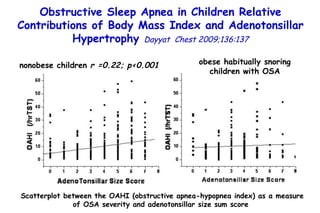
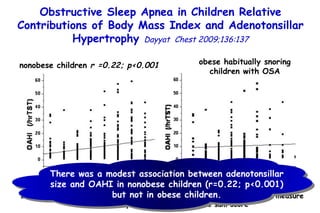
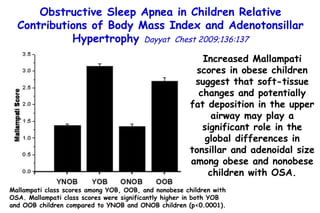
![Box plots of adenotonsillar size scores among young obese (YOB) and old obese (OOB) children and nonobese children. A denotonsillar size scores are significantly lower in both YOB and OOB children compared to their nonobese counterparts (young nonobese [YNO] and old nonobese [ONO]) [p<0.0001]. Obstructive Sleep Apnea in Children Relative Contributions of Body Mass Index and Adenotonsillar Hypertrophy Dayyat Chest 2009;136:137 Children with OSA Children with OAHI](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-486-320.jpg)
![Box plots of adenotonsillar size scores among young obese (YOB) and old obese (OOB) children and nonobese children. A denotonsillar size scores are significantly lower in both YOB and OOB children compared to their nonobese counterparts (young nonobese [YNO] and old nonobese [ONO]) [p<0.0001]. Obstructive Sleep Apnea in Children Relative Contributions of Body Mass Index and Adenotonsillar Hypertrophy Dayyat Chest 2009;136:137 Children with OSA Children with OAHI The magnitude of adenotonsillar hypertrophy required for any given magnitude of OAHI is more likely to be smaller in obese children compared to nonobese children.](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-487-320.jpg)


![Influenza Exerts Continued Pressure in an Era of Modern Medicine. Noah Am J Respir Cell Mol Biol 2009;41:3 Influenza particles are spherical (~ 100 nm diameter), with a lipid bilayer derived from the host plasma membrane. The virion contains a matrix protein (M1) and three transmembrane proteins (hemagglutinin [HA] and neuraminidase [NA]), which are the major antigenic determinants, and a small membrane-bound protein (M2). Beneath the matrix coat is the helical ribonucleocapsid, which includes the vRNA genome, nucleoprotein (NP), nuclear export protein (NEP), and the three viral polymerase subunits (PB1, PB2, PA). THE INFLUENZA REPLICATION CYCLE, SHIFT, AND DRIFT](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-552-320.jpg)
![Influenza Exerts Continued Pressure in an Era of Modern Medicine. Noah Am J Respir Cell Mol Biol 2009;41:3 Influenza particles are spherical (~ 100 nm diameter), with a lipid bilayer derived from the host plasma membrane. The virion contains a matrix protein (M1) and three transmembrane proteins (hemagglutinin [HA] and neuraminidase [NA]), which are the major antigenic determinants, and a small membrane-bound protein (M2). Beneath the matrix coat is the helical ribonucleocapsid, which includes the vRNA genome, nucleoprotein (NP), nuclear export protein (NEP), and the three viral polymerase subunits (PB1, PB2, PA). There are 16 different HA, and nine different NAs. THE INFLUENZA REPLICATION CYCLE, SHIFT, AND DRIFT](https://image.slidesharecdn.com/w2010pulmonology-100524110112-phpapp02/85/Pulmonology-553-320.jpg)