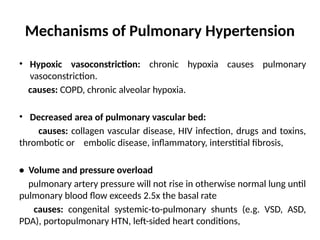
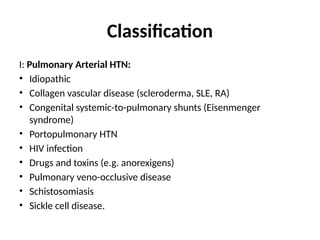
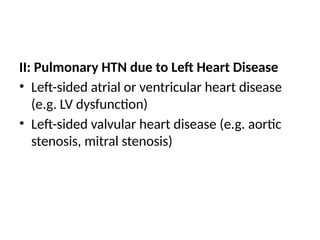
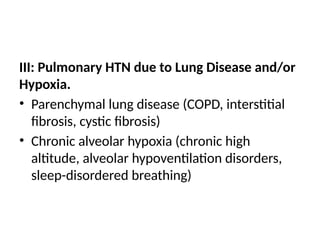
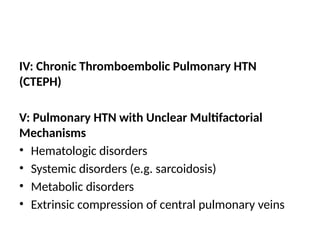
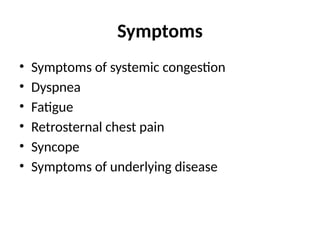
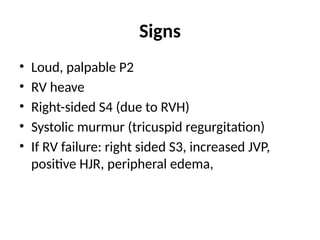
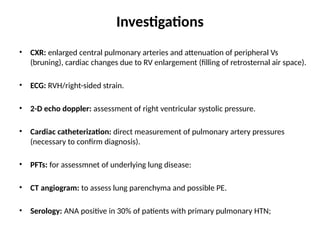
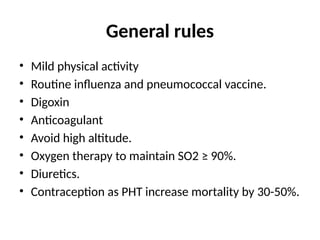
Pulmonary hypertension is defined by a mean pulmonary arterial pressure above 25 mmHg. It can arise from various mechanisms, including hypoxic vasoconstriction, left heart disease, lung disease, and chronic thromboembolic events, with various classification types and symptoms such as dyspnea and fatigue. Diagnosis involves imaging and catheterization, and treatment options include medications like CCBs and prostanoids, or lung transplantation in severe cases.