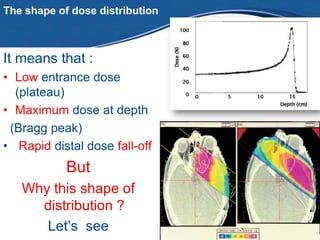
Proton therapy is able to more precisely target radiation dose to tumor tissues while minimizing dose to surrounding healthy tissues. Photon therapy deposits radiation throughout the tissues it passes through, whereas proton therapy deposits most of its energy at a specific depth called the Bragg peak. This allows protons to deliver a high radiation dose to the tumor with little exit dose, improving treatment of cancers near critical structures.