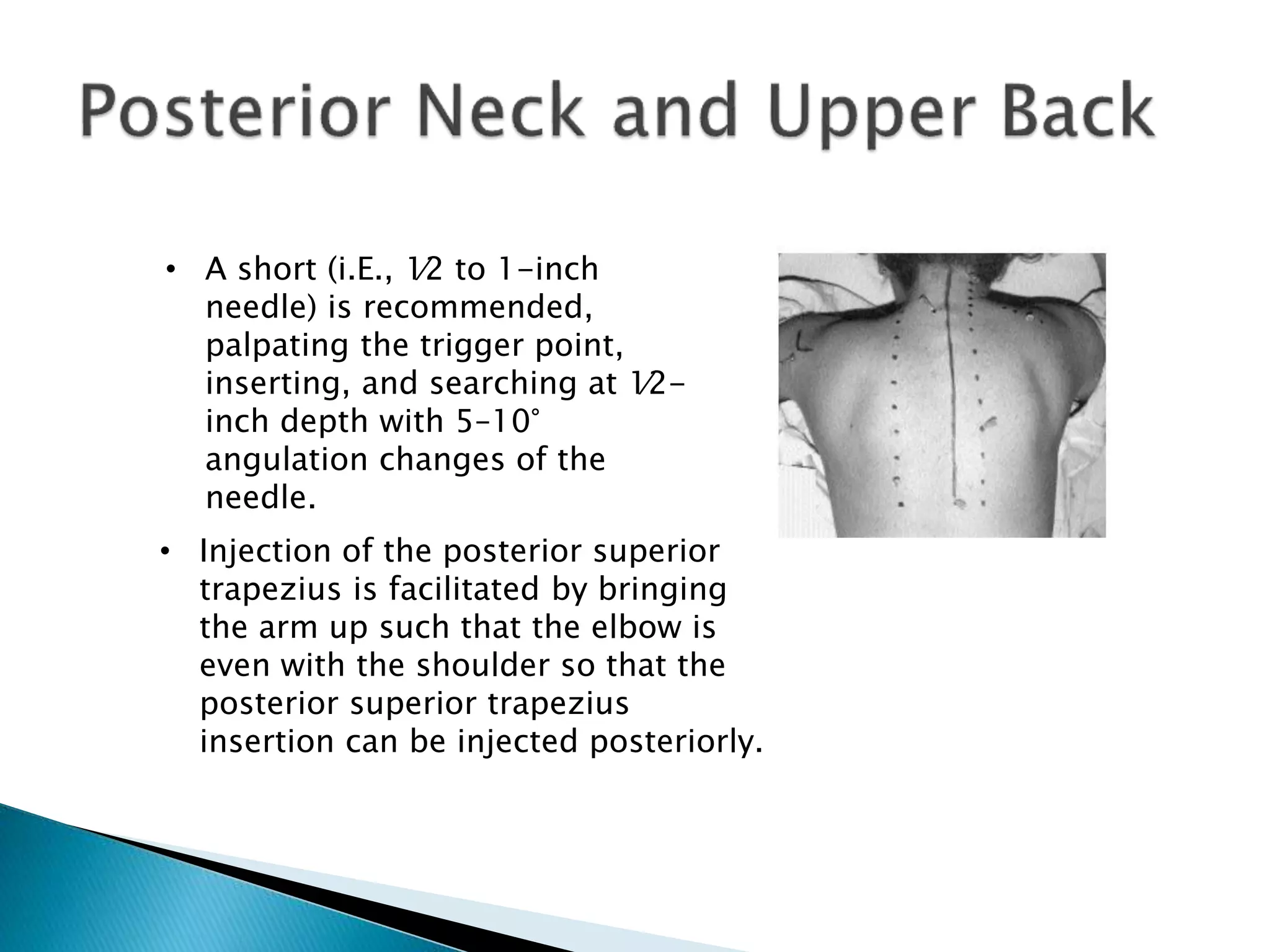
This document provides an overview of prolotherapy. It begins with definitions and explanations of prolotherapy, noting it involves injecting irritants like dextrose to promote new tissue growth. It describes the mechanism of action as causing a healing cascade through inflammation. It outlines candidate selection criteria, common indications, contraindications, complications, treatment course and evidence from studies showing benefits for pain reduction and improved function. The document provides details on various proliferant solutions, injection sites, and references several studies supporting the use and effectiveness of prolotherapy.