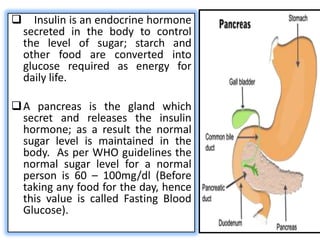
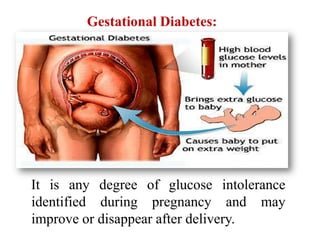
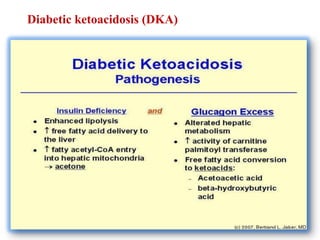
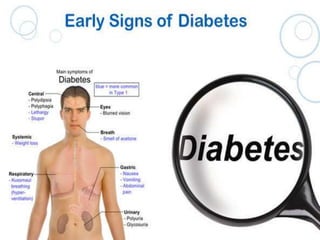
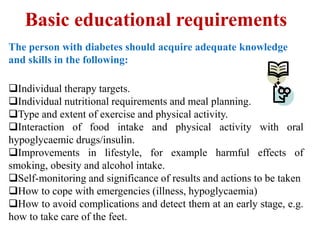
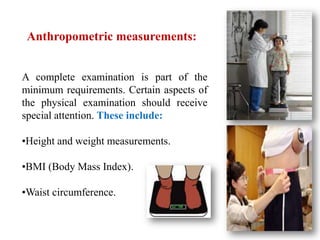
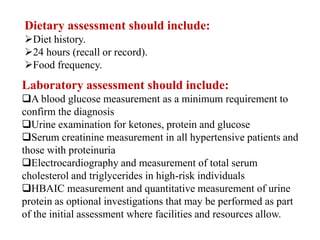
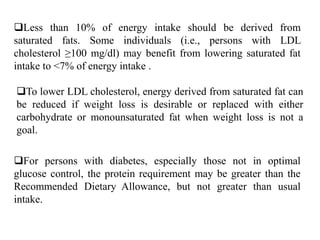
The document provides an overview of the history, definitions, classifications, signs and symptoms, complications, diagnosis, treatment, and management of diabetes mellitus. It discusses the role of insulin and pancreas in regulating blood sugar levels and classifies diabetes into types 1, 2, gestational, and pre-diabetes. The document also outlines dietary, exercise, medication-based, and self-management recommendations for diabetes.