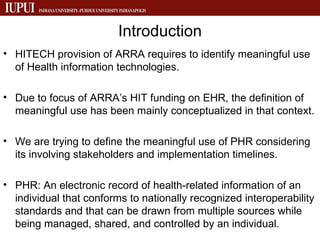
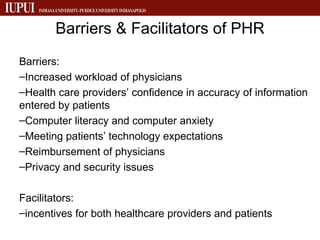
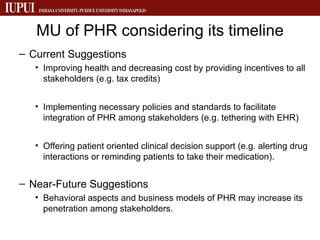
The document discusses the meaningful use of personal health records (PHRs) in the context of healthcare technology, emphasizing the need to define its usage amidst various stakeholders. It identifies barriers such as physician workload and privacy concerns, alongside facilitators like incentives for healthcare providers and patients. Suggestions for improving PHR utilization include implementing supportive policies, integrating genomic data, and enhancing patient engagement through technology.