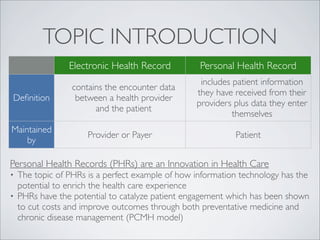
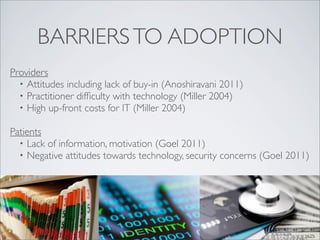
Personal health records (PHRs) enhance patient engagement and improve health outcomes while potentially reducing costs in healthcare. Key stakeholders, including patients, providers, and payers, can benefit from PHRs, although various barriers such as technology adoption and security concerns exist. To maximize the effectiveness of PHRs, it's essential to focus on user-friendly design, regulatory support, and addressing both patient and provider needs.