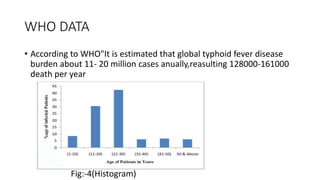
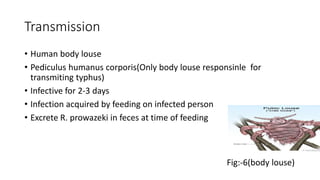
Typhus fever is caused by Rickettsia bacteria and is transmitted by body lice. It includes epidemic typhus caused by R. prowazekii and transmitted by body lice. According to WHO, there are an estimated 11-20 million cases of typhoid fever annually resulting in 128,000-161,000 deaths per year. Typhus fever most commonly occurs in people living in unhygienic conditions such as refugee camps or mountainous regions. The bacteria are transmitted through the feces of infected body lice. Symptoms include high fever, headache, muscle pain and rash. Treatment involves antibiotics such as doxycycline. Prevention focuses on proper hygiene, disposal of waste,