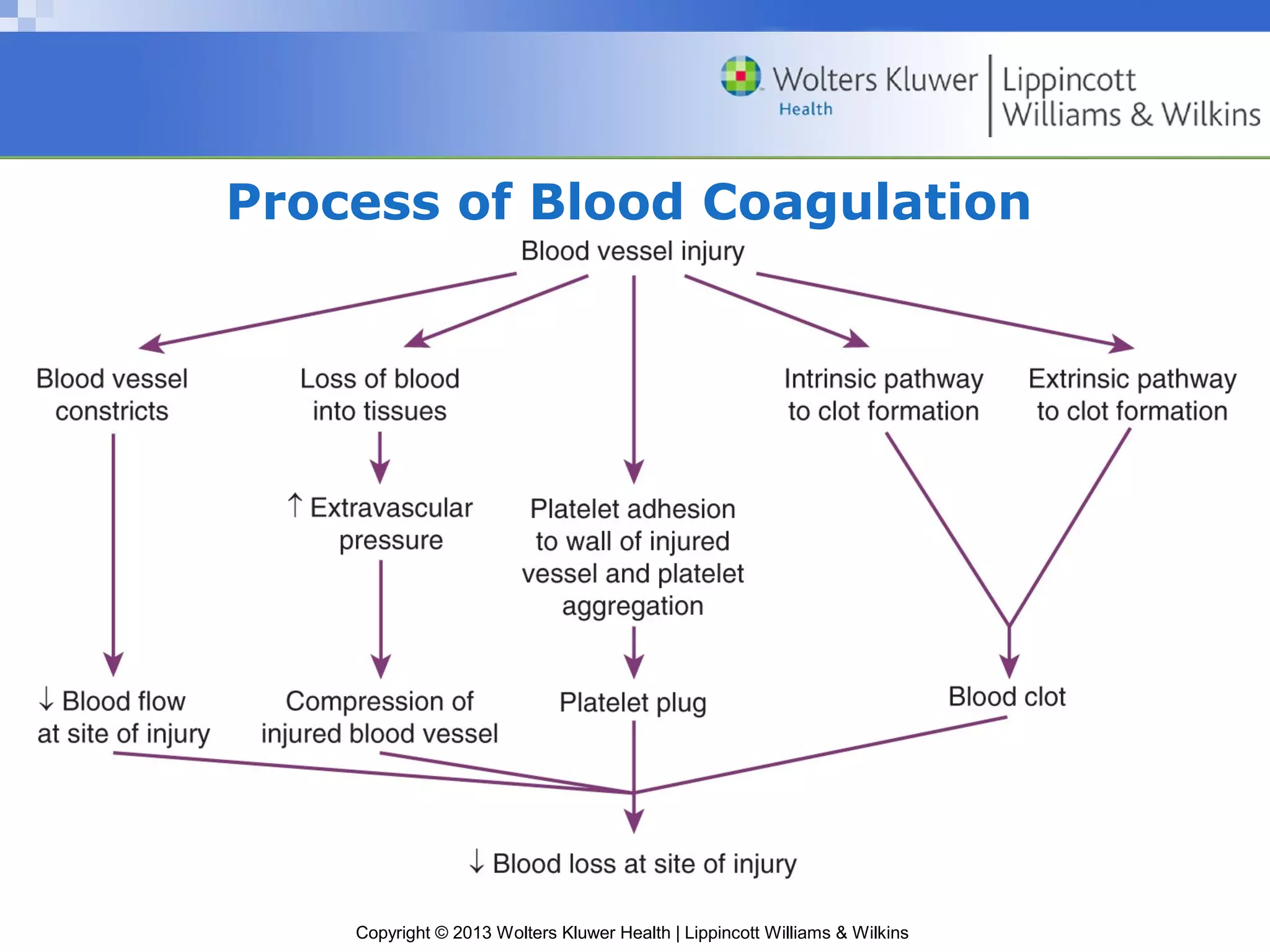
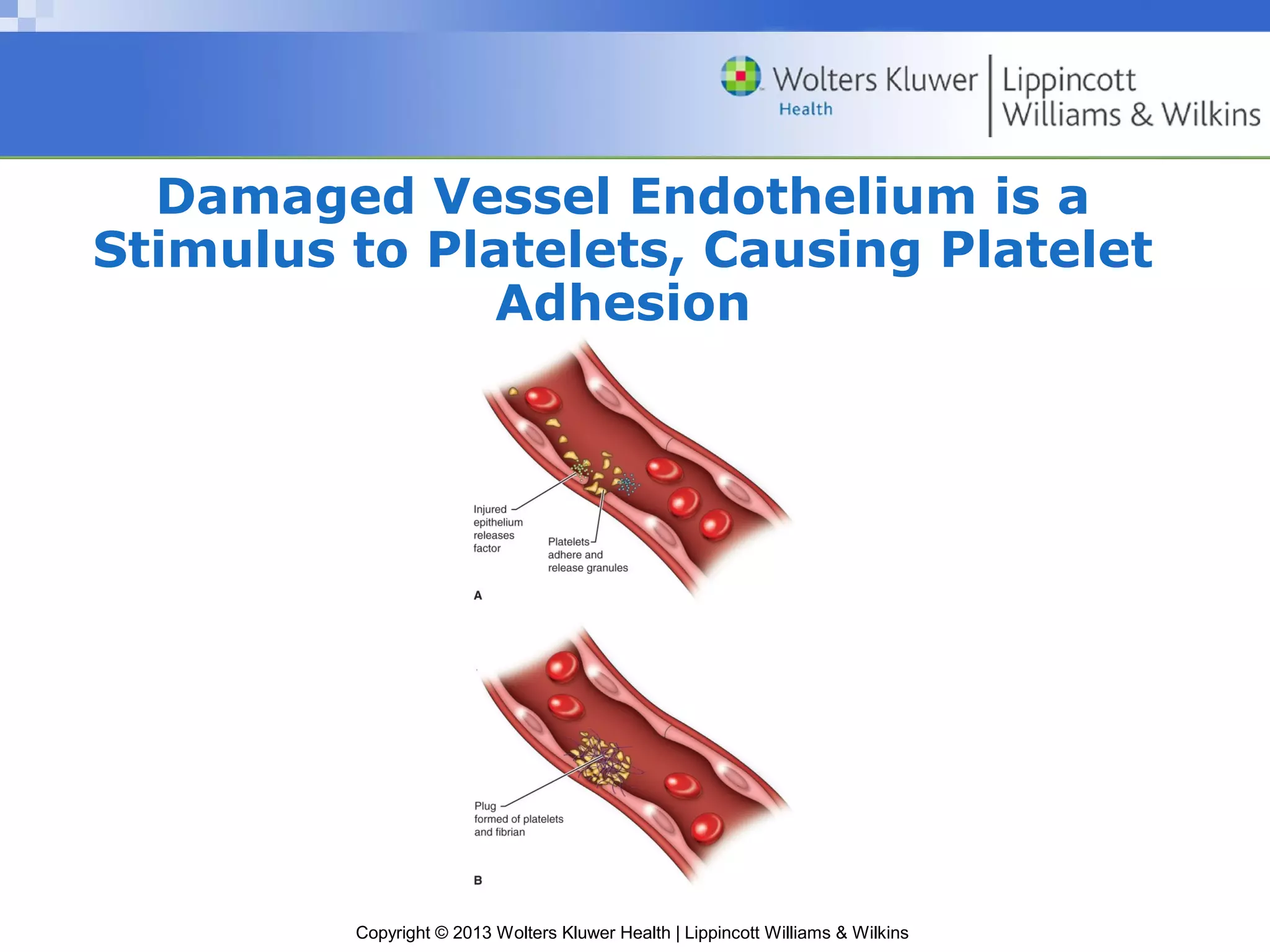
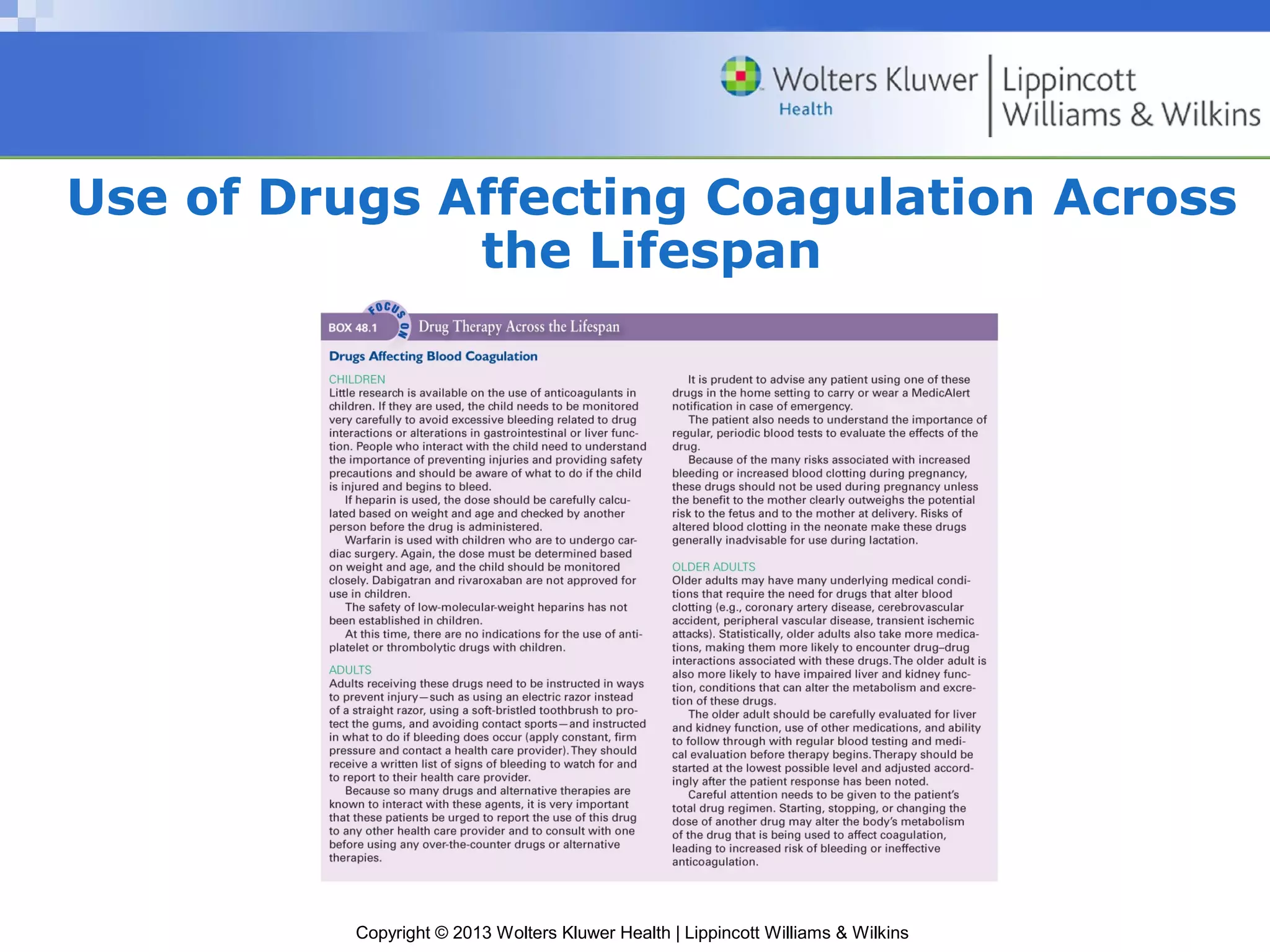
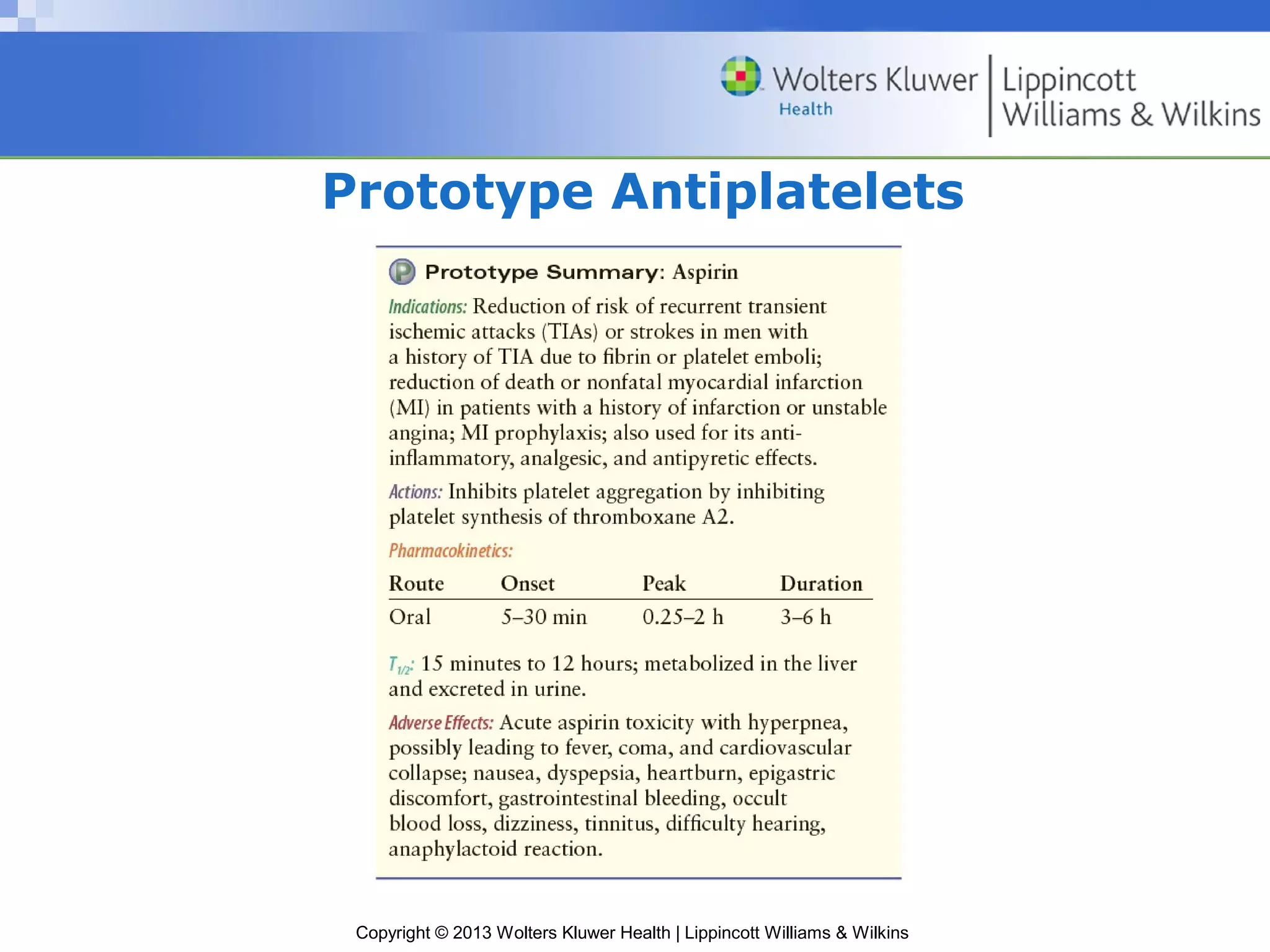
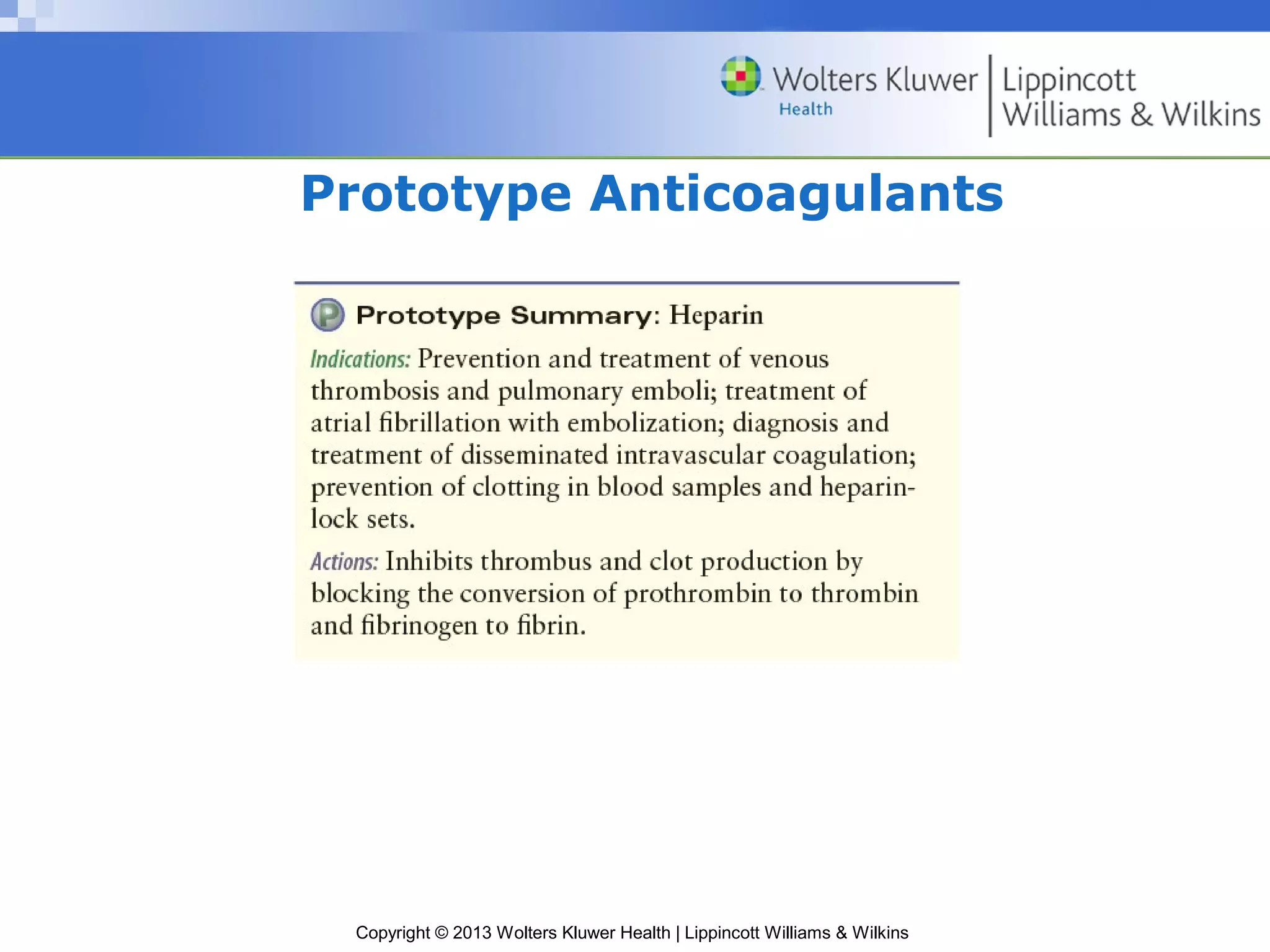
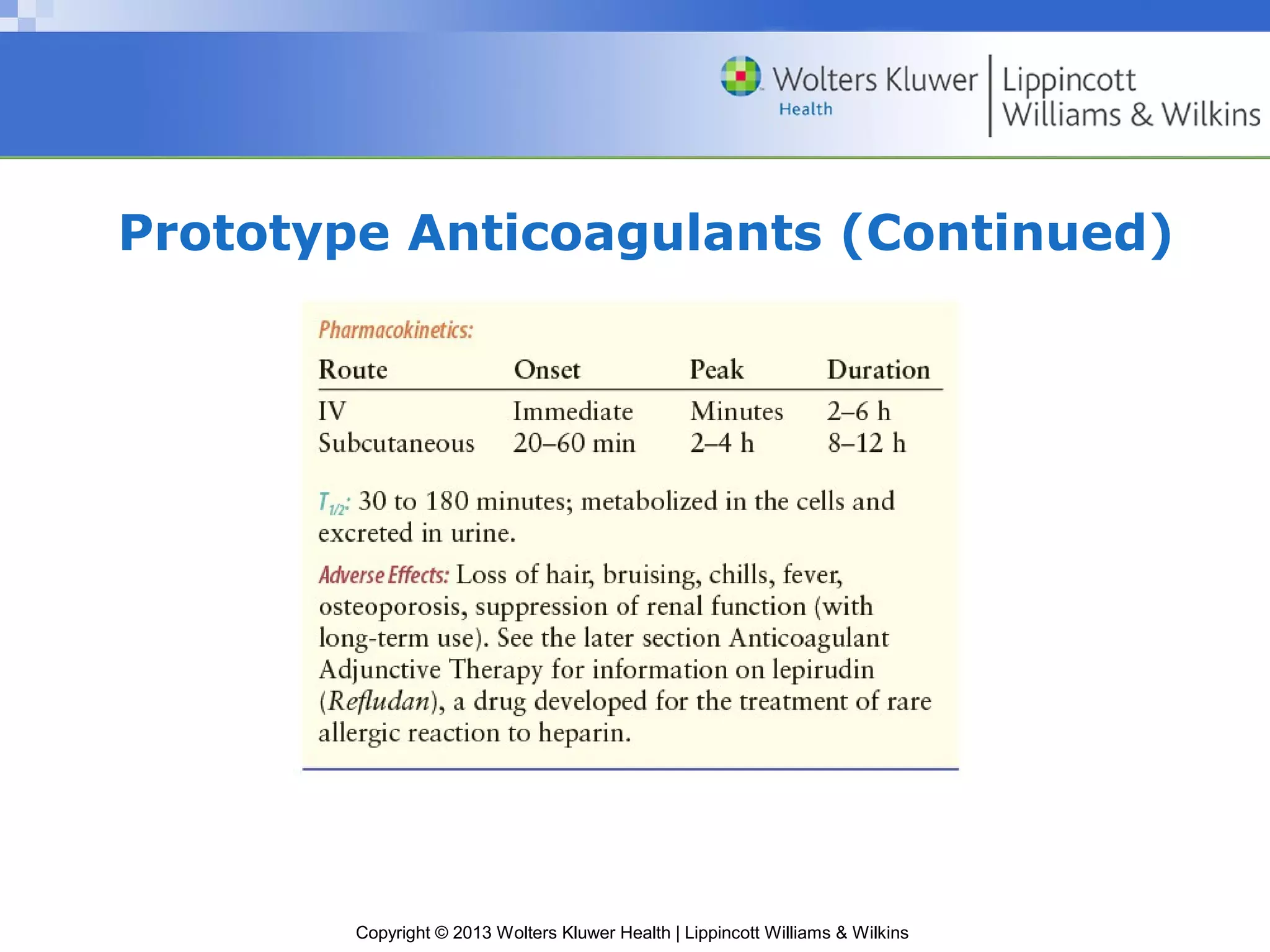
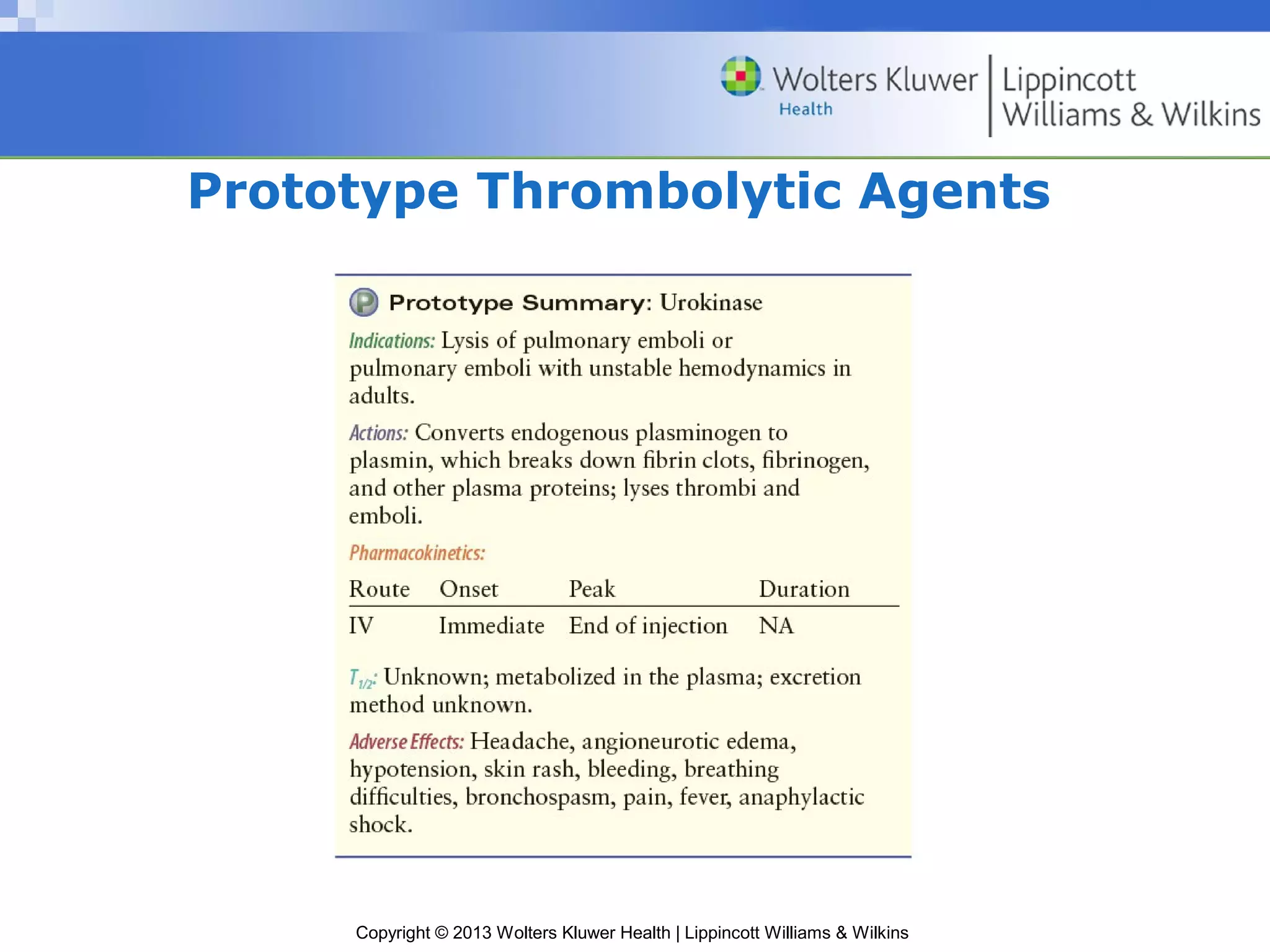
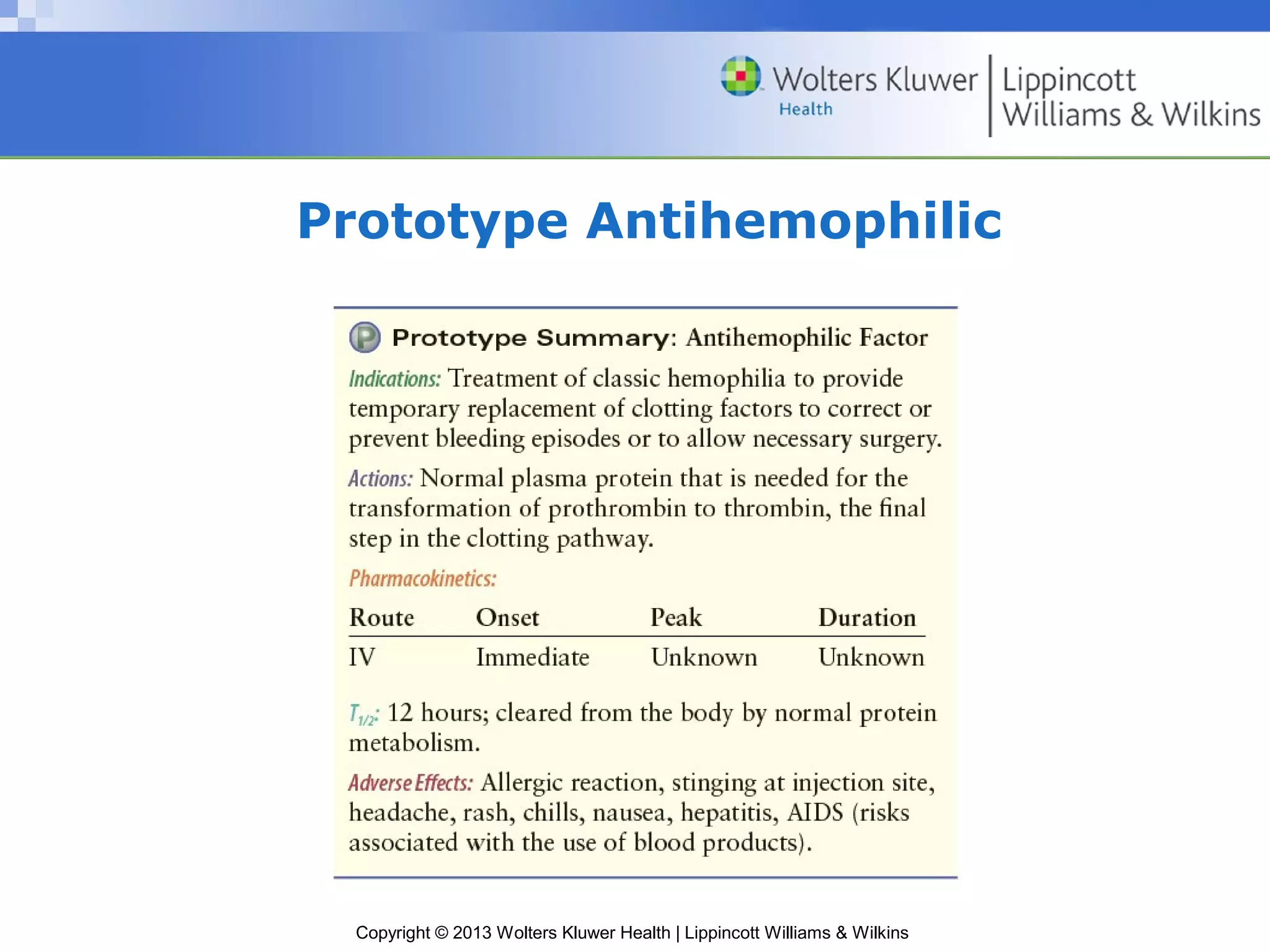
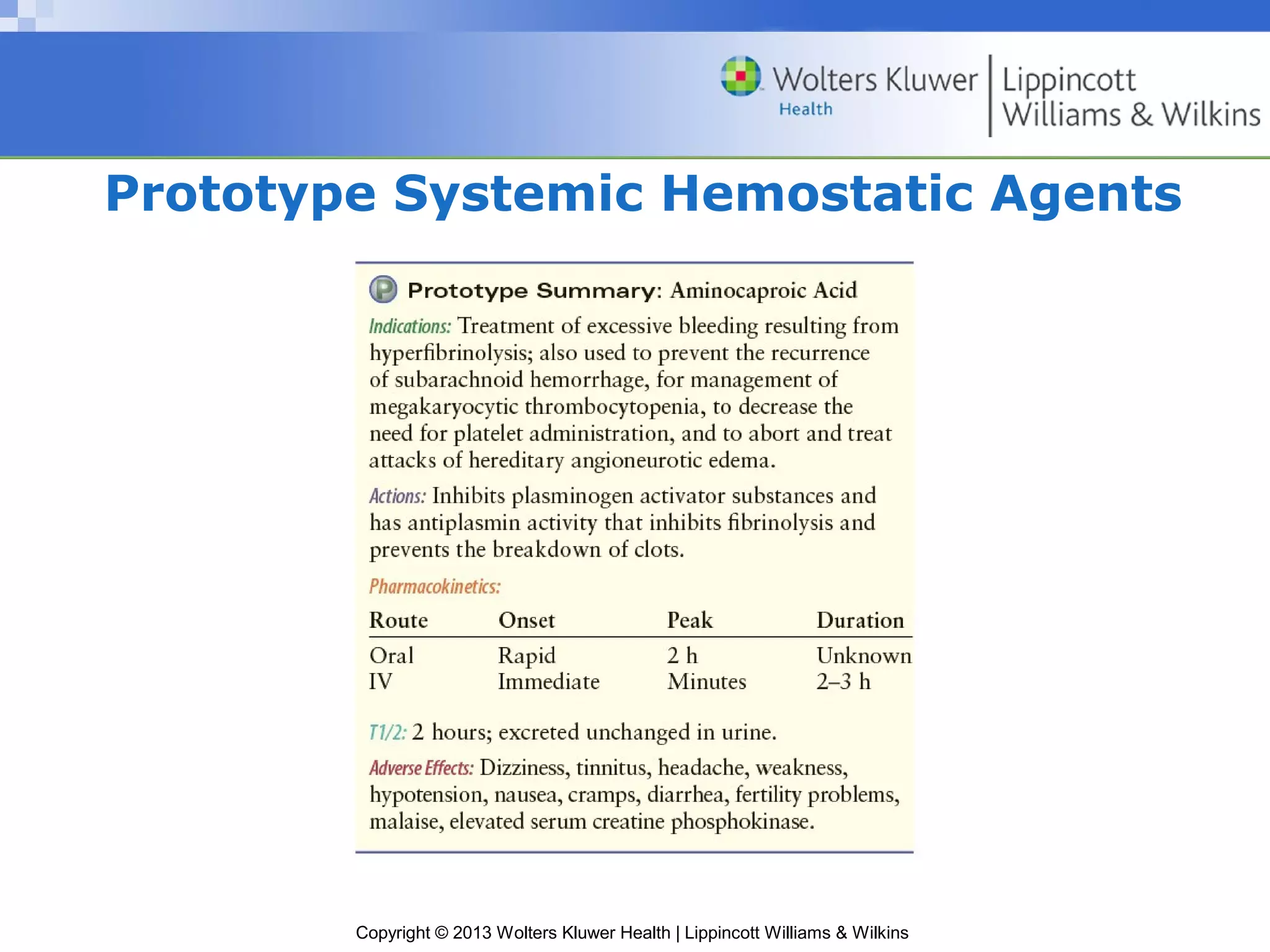
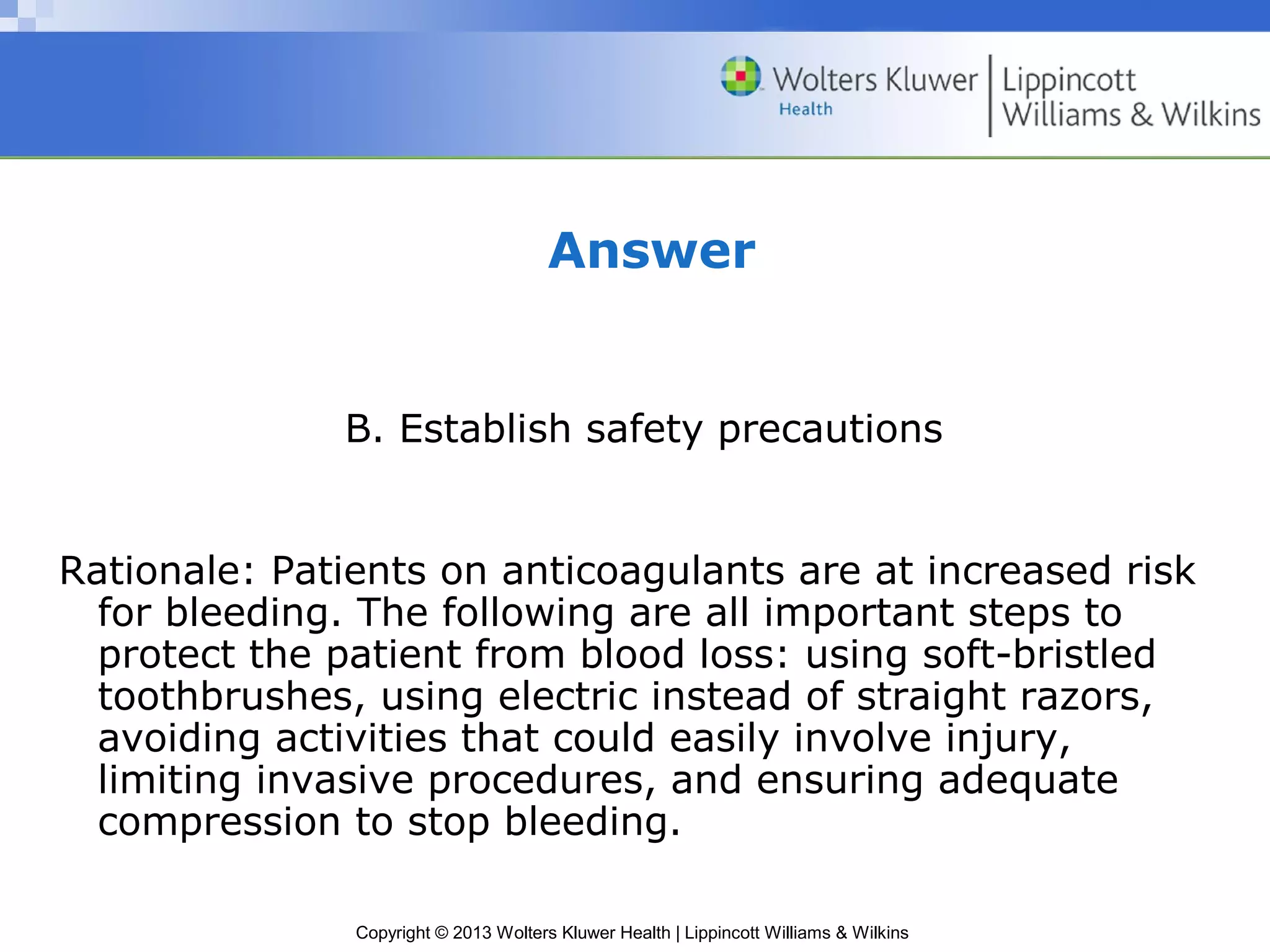
The document discusses drugs that affect blood coagulation, including antiplatelets, anticoagulants, thrombolytic agents, antihemophilic factors, and systemic hemostatic agents. It describes the mechanisms of action, indications, pharmacokinetics, cautions, adverse effects, and drug interactions of these drug classes and provides examples of prototype drugs within each class. It also discusses the coagulation process and disorders like thrombosis, hemorrhage, and bleeding disorders.