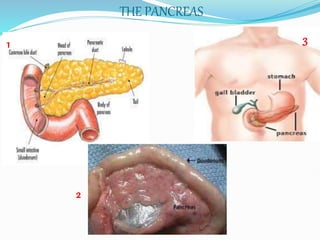
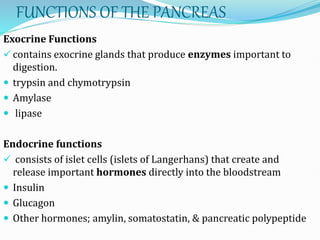
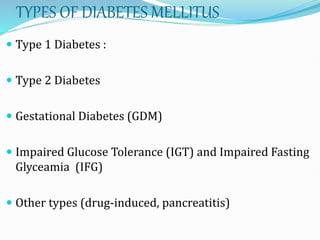
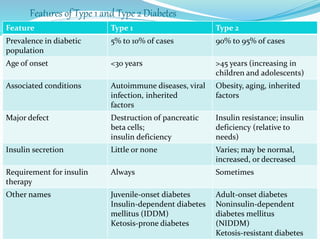
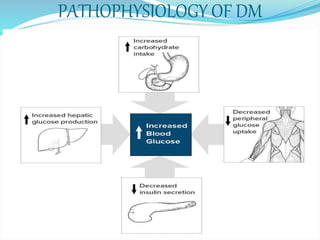
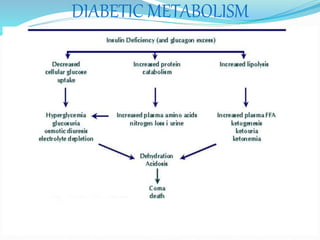
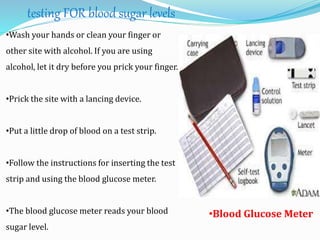
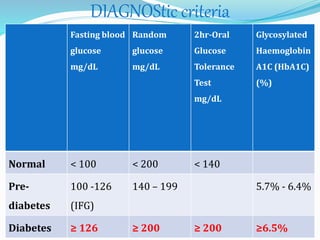
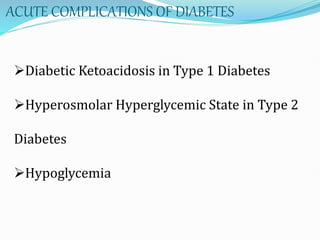
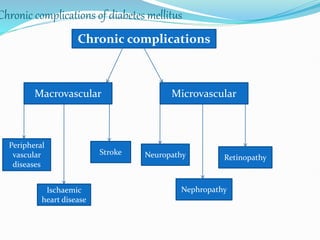
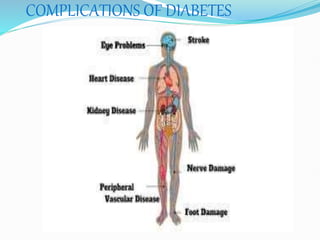
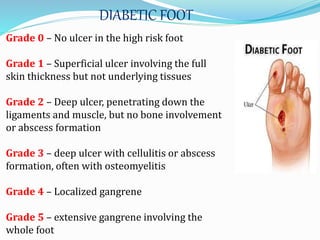
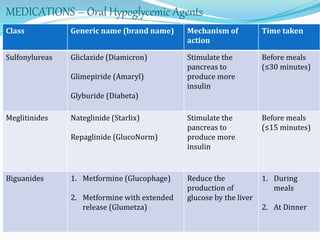
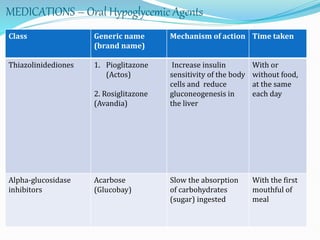
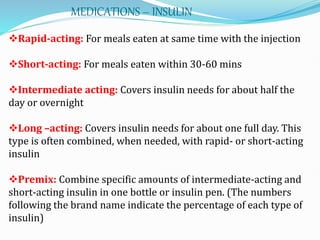
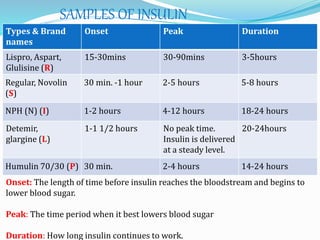
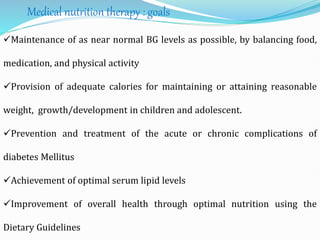
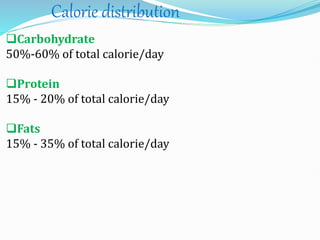
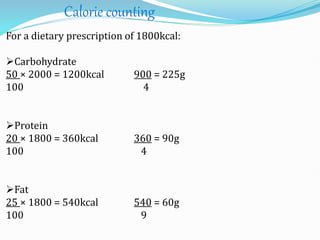
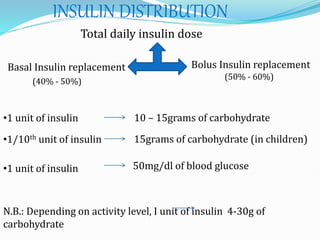
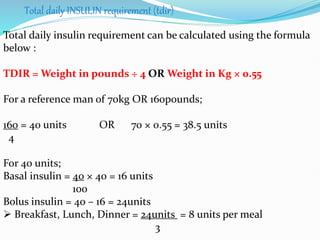
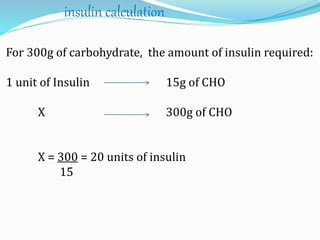
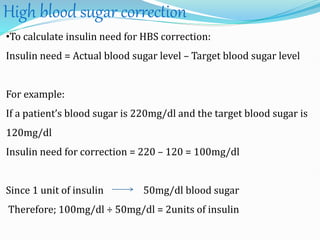
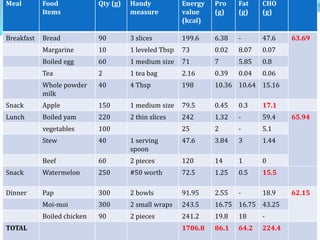
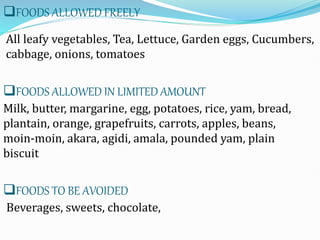
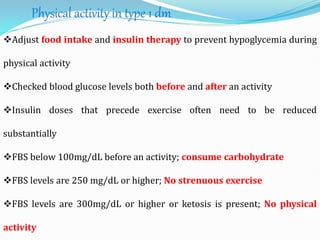
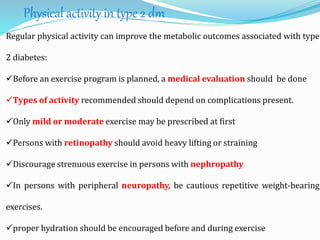
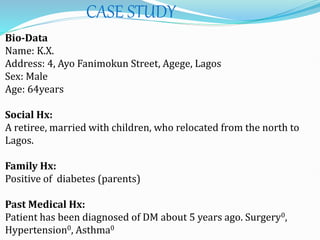
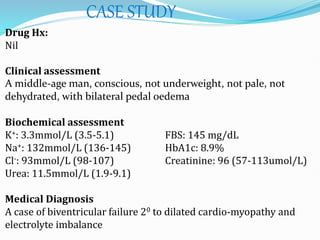
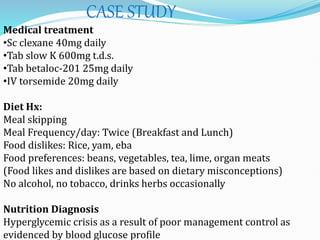
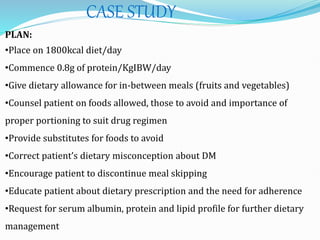
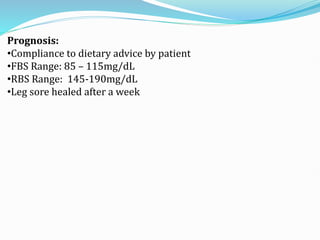
The document outlines diabetes mellitus, covering its definition, prevalence, types, symptoms, and management strategies. It highlights the increasing global prevalence, the role of the pancreas in insulin production, and the various medications and dietary approaches for diabetes management. Additionally, it includes a case study emphasizing the importance of personalized dietary plans and adherence to treatment for better health outcomes.