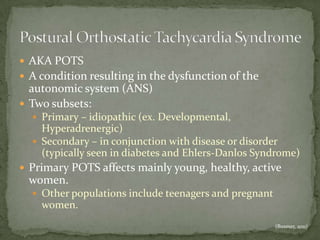
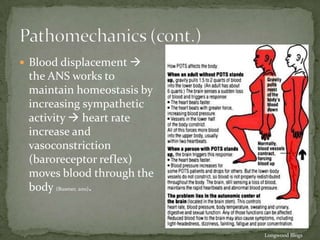
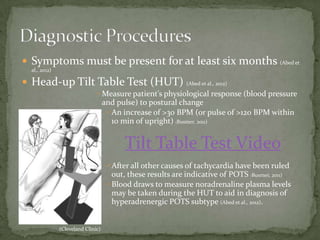
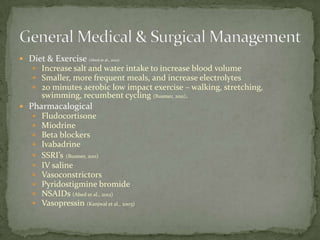
The document discusses postural orthostatic tachycardia syndrome (POTS), a condition caused by dysautonomia or malfunction of the autonomic nervous system. POTS results in an excessive increase in heart rate when standing up. It most often affects young, healthy women and can be primary (idiopathic) or secondary, associated with other diseases. Symptoms include dizziness, palpitations, and fatigue. Diagnosis involves documenting an increased heart rate above 30 bpm within 10 minutes of standing via tilt table testing. Treatment focuses on lifestyle changes, medication, and physical countermeasures to increase blood volume and improve symptoms.