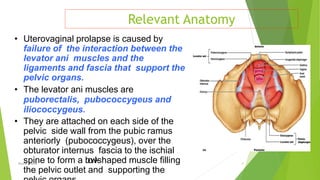
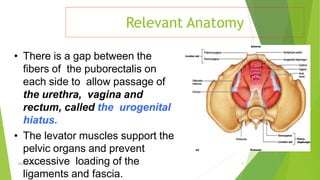
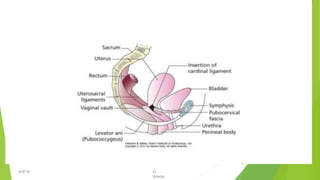
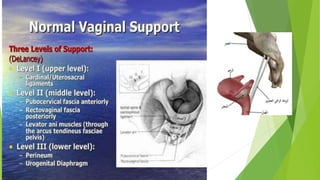
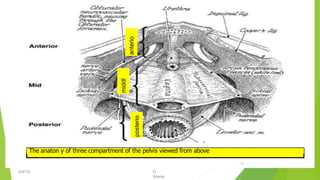
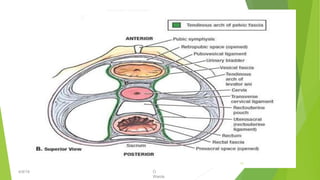
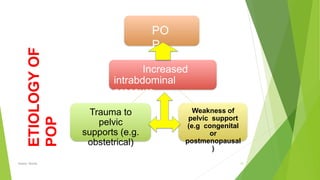
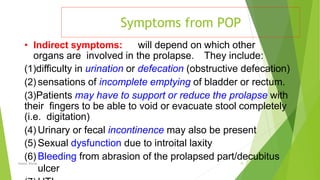
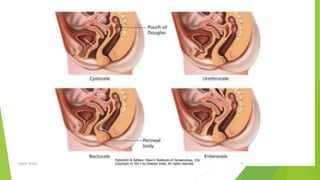
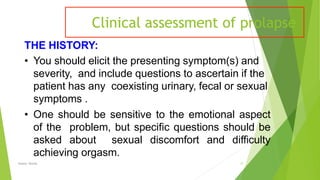
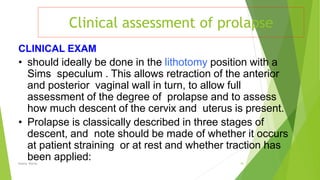
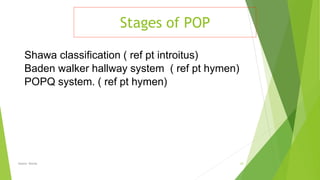
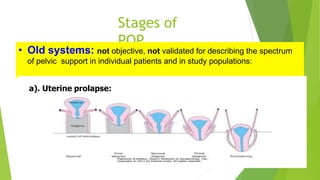
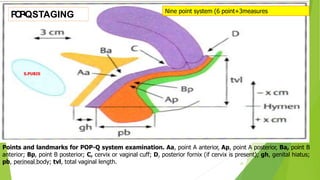
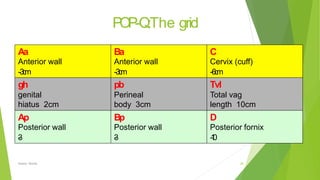
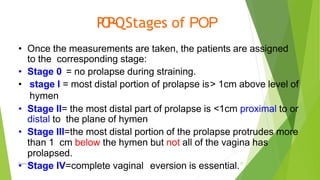
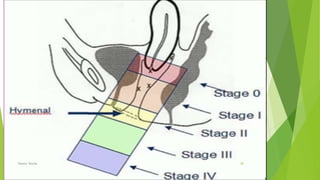
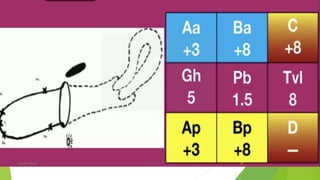
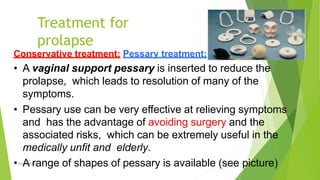
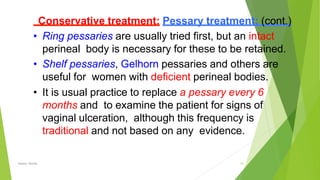
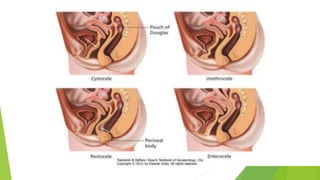
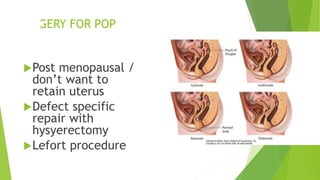
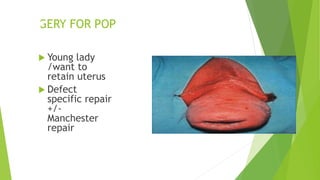
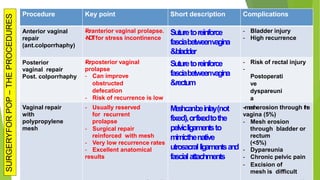
Pelvic organ prolapse (POP) occurs when pelvic organs such as the bladder, uterus, or rectum descend from their normal positions due to weakness in the muscles and tissues that support them. Symptoms may include a sensation of bulging or pressure in the vagina. POP has stages from I to IV depending on how far the organs have descended. Treatment options include pelvic floor exercises, pessaries to support organs, or surgery to repair tissues. Surgical procedures aim to restore normal anatomy and are defect-specific depending on the affected compartment. While surgery effectively treats POP, recurrence rates are around 5% and mesh procedures carry risks of erosion or pain.