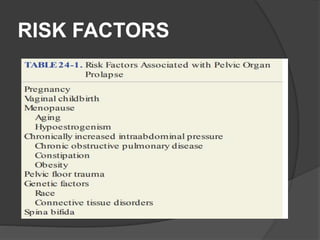
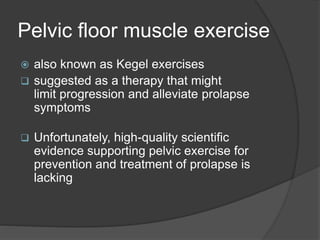
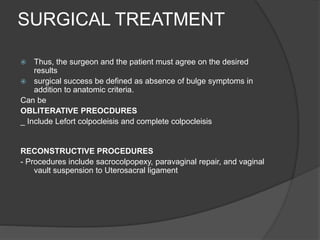
Pelvic organ prolapse is a common condition that can diminish quality of life. Signs include descent of the anterior vaginal wall, posterior vaginal wall, uterus, vaginal apex or perineum. Symptoms include vaginal bulging, pelvic pressure and splinting. Risk factors include vaginal childbirth. Treatment options include expectant management, pessaries, pelvic floor exercises, and surgery. Surgical options range from obliterative procedures that close the vagina to reconstructive procedures like sacrocolpopexy that repair prolapse.