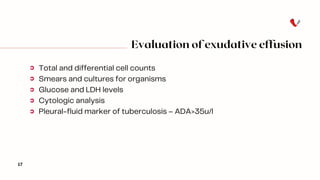
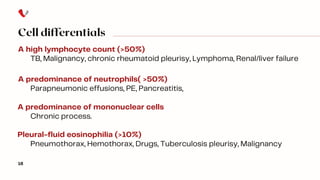
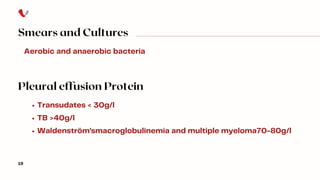
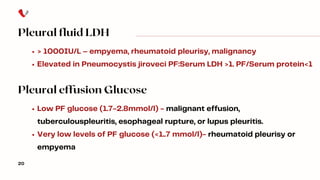
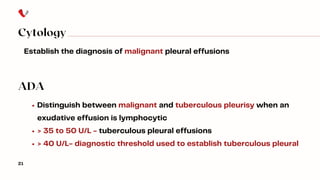
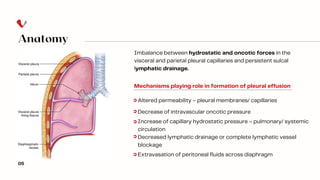
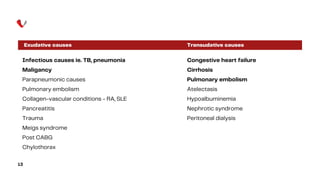
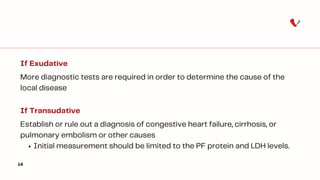
The document discusses pleural effusion, a pathological accumulation of fluid in the pleural space often resulting from cardiovascular or inflammatory conditions. It outlines the clinical presentation, necessary workups including thoracentesis, and differentiates between transudative and exudative effusions based on specific criteria. The document emphasizes the importance of biochemical and cytological analysis to determine the underlying causes of pleural effusions.


![Distinguishing Transudates From Exudates
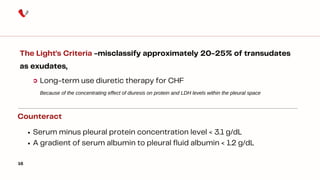
The Light's Criteria -measures serum and pleural fluid protein and LDH
15
Pleural fluid protein/serum protein ratio greater than 0.5, or
Pleural fluid LDH/serum LDH ratio greater than 0.6, or
Pleural fluid LDH greater than two-thirds the upper limits of the
laboratory's normal serum LDH
Light's criteria yield a 97.5% sensitivity and 80% specificity.
[Reappraisal of the standard method (Light's criteria) for identifying pleural exudates]. 2006,José M Porcel et al](https://image.slidesharecdn.com/pleuralfluidanalysis-241025125556-3c4accf6/85/Pleural-fluid-analysis-Approach-Body-fluid-analysis-15-320.jpg)