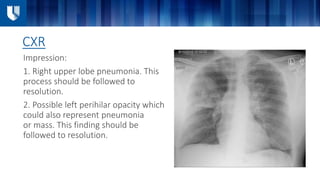
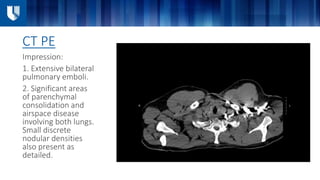
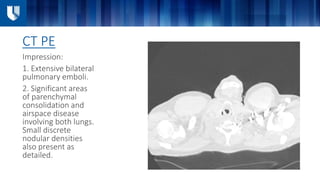
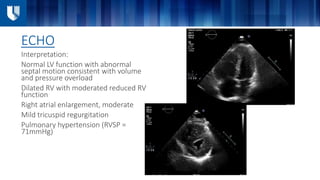
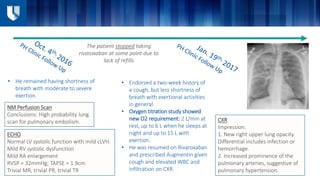
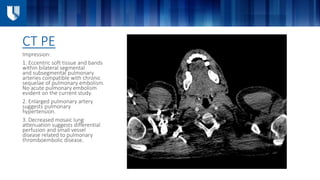
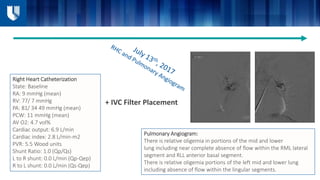
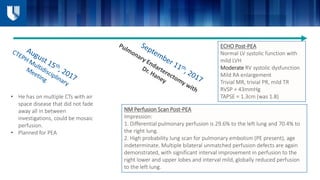
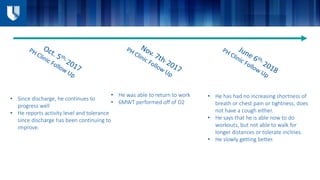
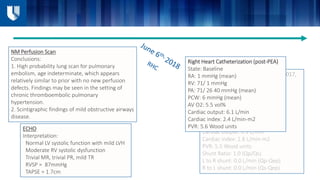
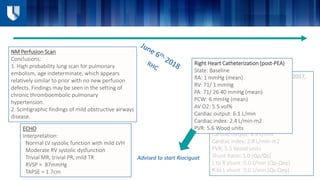
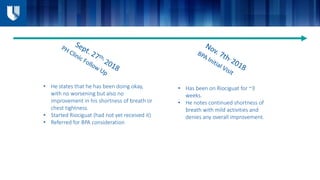
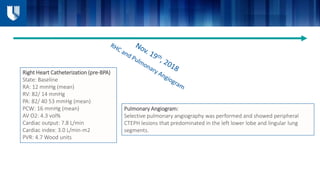
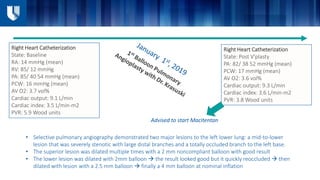
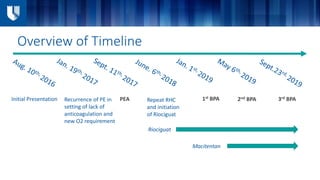
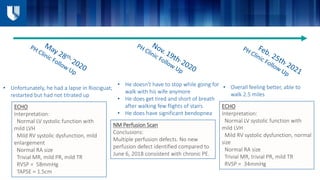
The patient initially presented with pulmonary embolism and was treated with anticoagulation and antibiotics for pneumonia, but developed recurrent symptoms of pulmonary hypertension. After pulmonary endarterectomy, the patient still had elevated pulmonary pressures and was started on Riociguat, but had no improvement. Right heart catheterization showed ongoing pulmonary hypertension, so the patient underwent balloon pulmonary angioplasty of lesions in the left lower lobe, followed by initiation of Macitentan.