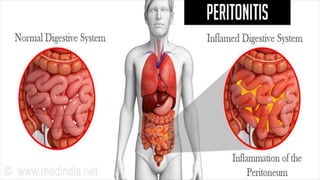
This document provides an overview of peritonitis, including:
- A case study of a 42-year-old male presenting with worsening abdominal pain, nausea and vomiting. Examination revealed abdominal guarding and tenderness.
- The main paths that can lead to peritonitis, including GI perforation, bacterial translocation, exogenous contamination, and female genital infections.
- The most common microbiology involves gram-negative bacteria and Clostridium perfringens.
- Clinical features include abdominal pain, constitutional symptoms, GI upset, elevated pulse, and abdominal tenderness. Investigations and management are also outlined.