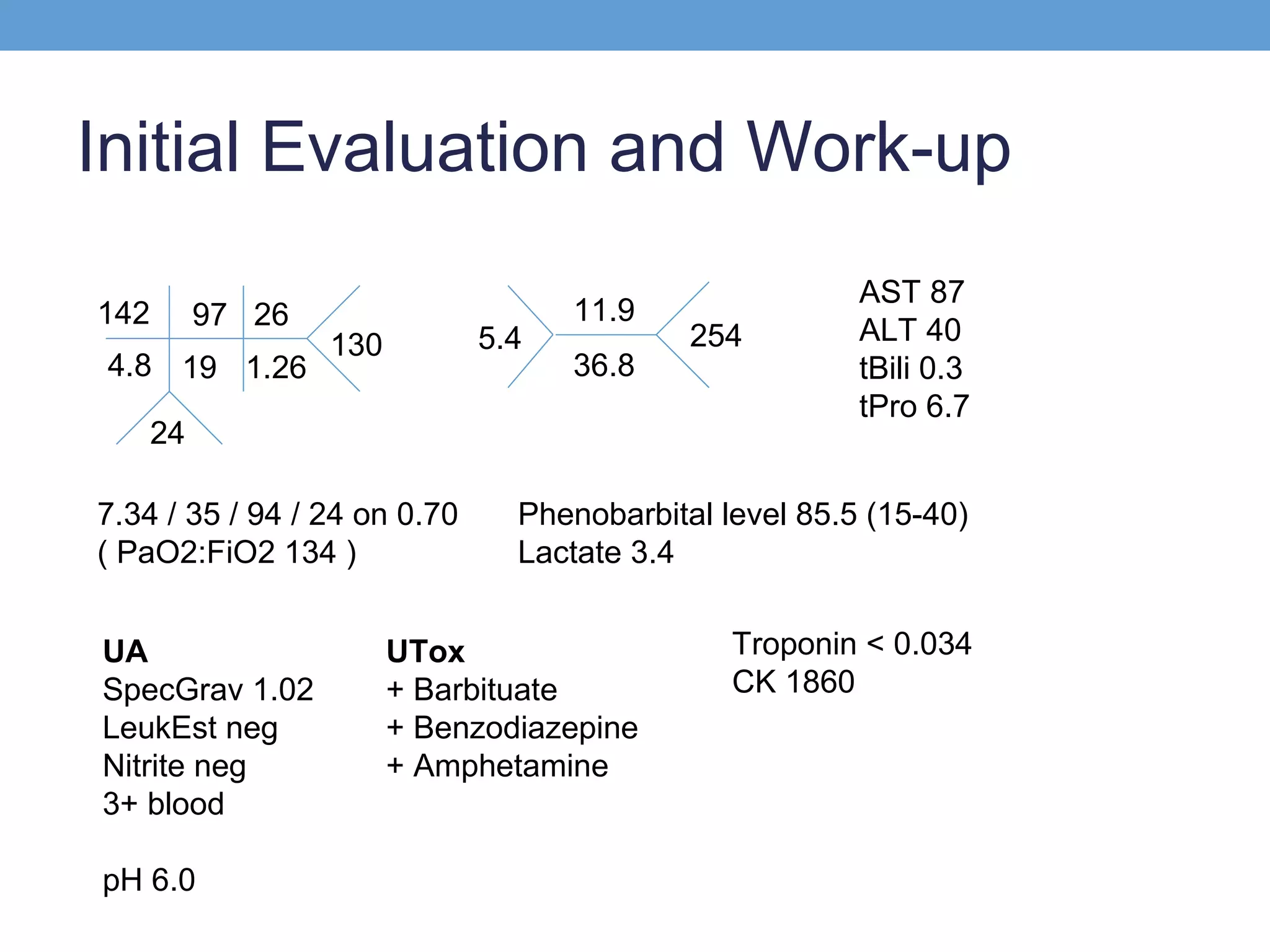
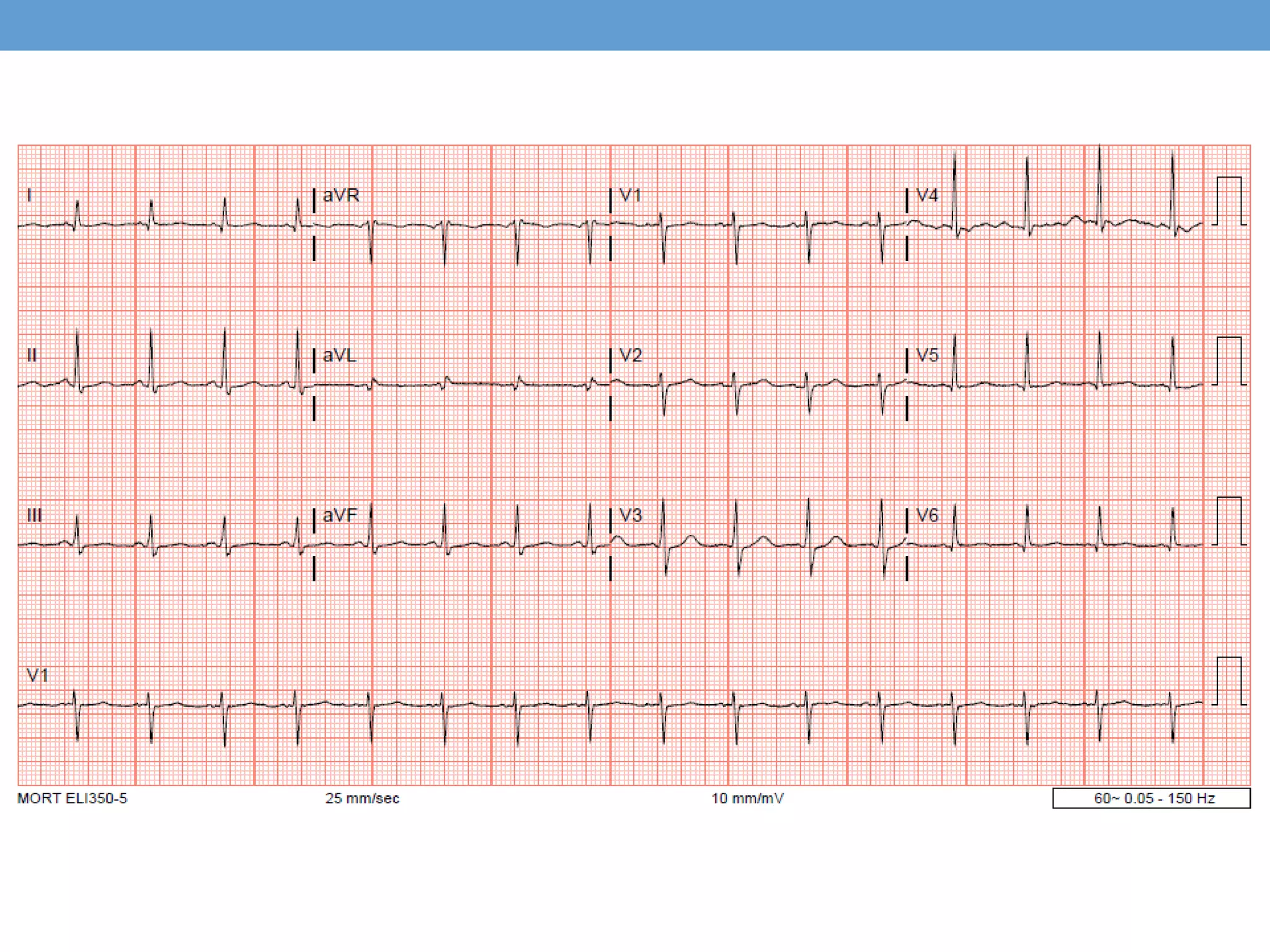
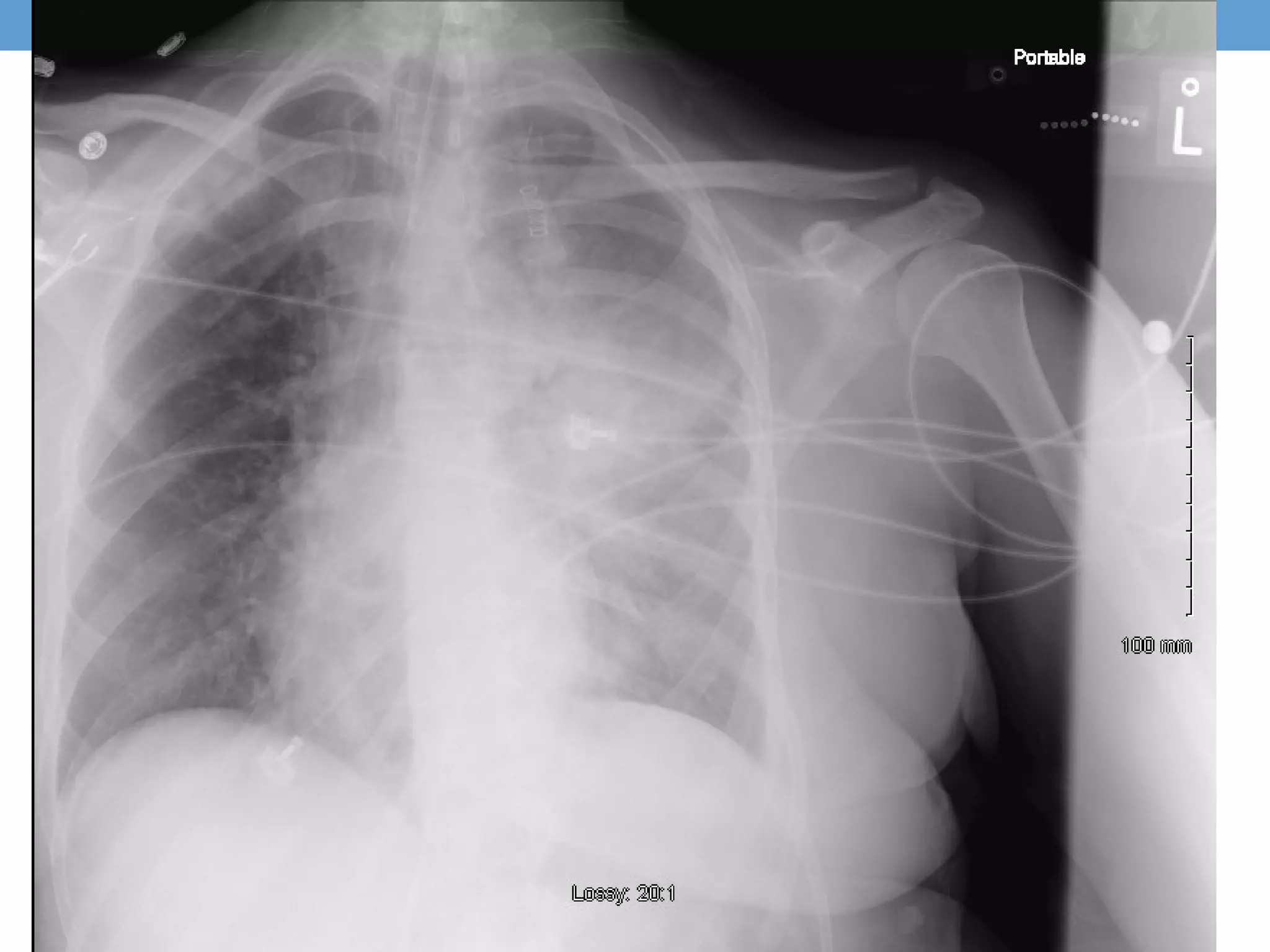
This patient presented with altered mental status and was found to have multiple substance intoxications. She was intubated and admitted to the ICU. Imaging revealed a saddle pulmonary embolism with right heart strain. Despite aggressive supportive care including anticoagulation, thrombolysis was administered with little benefit. Her condition continued to decline and she was transferred for possible surgical thrombectomy but continued supportive care. Pulmonary embolism should be considered in cases of unexplained cardiogenic shock.
![Objective
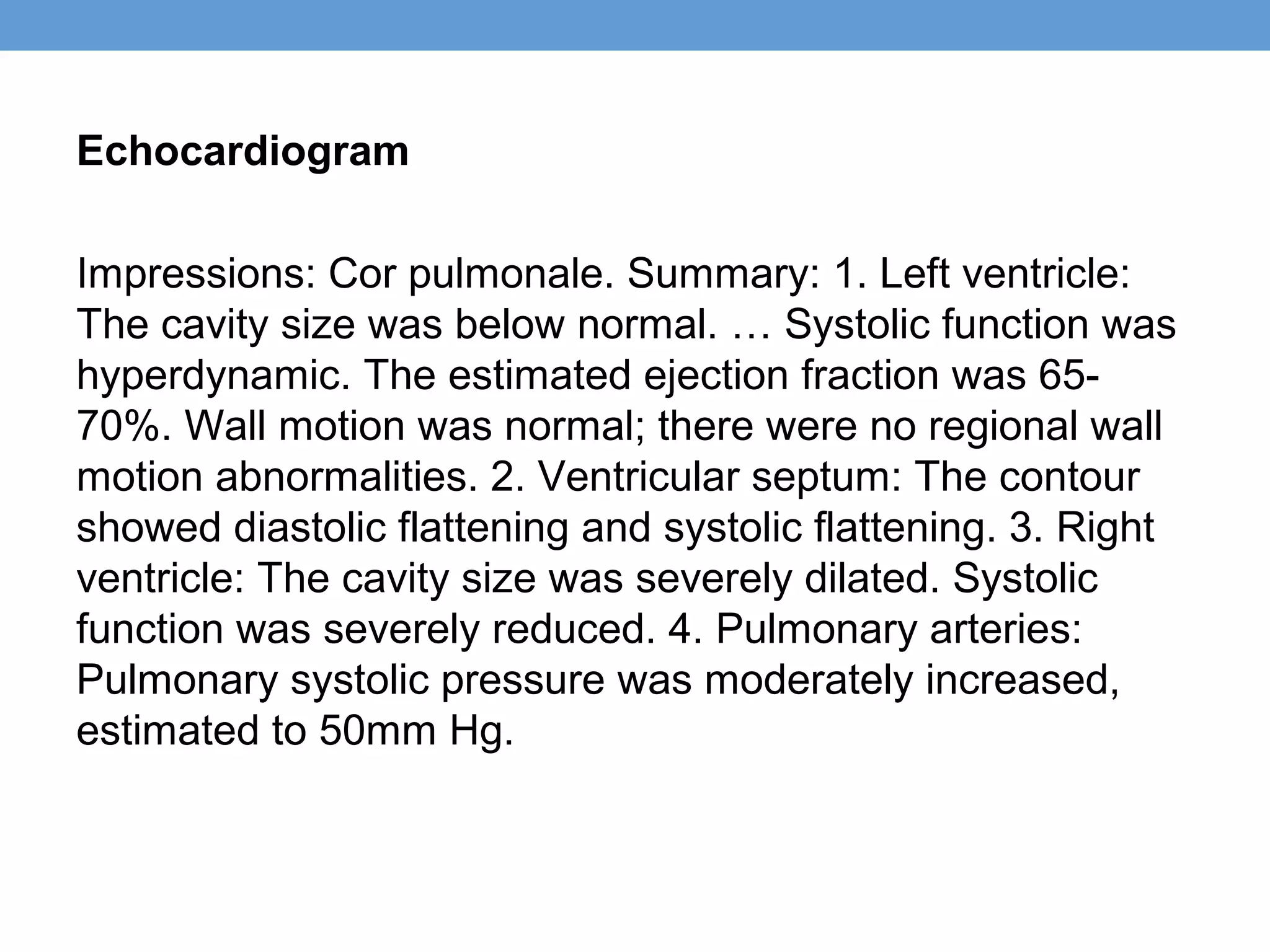
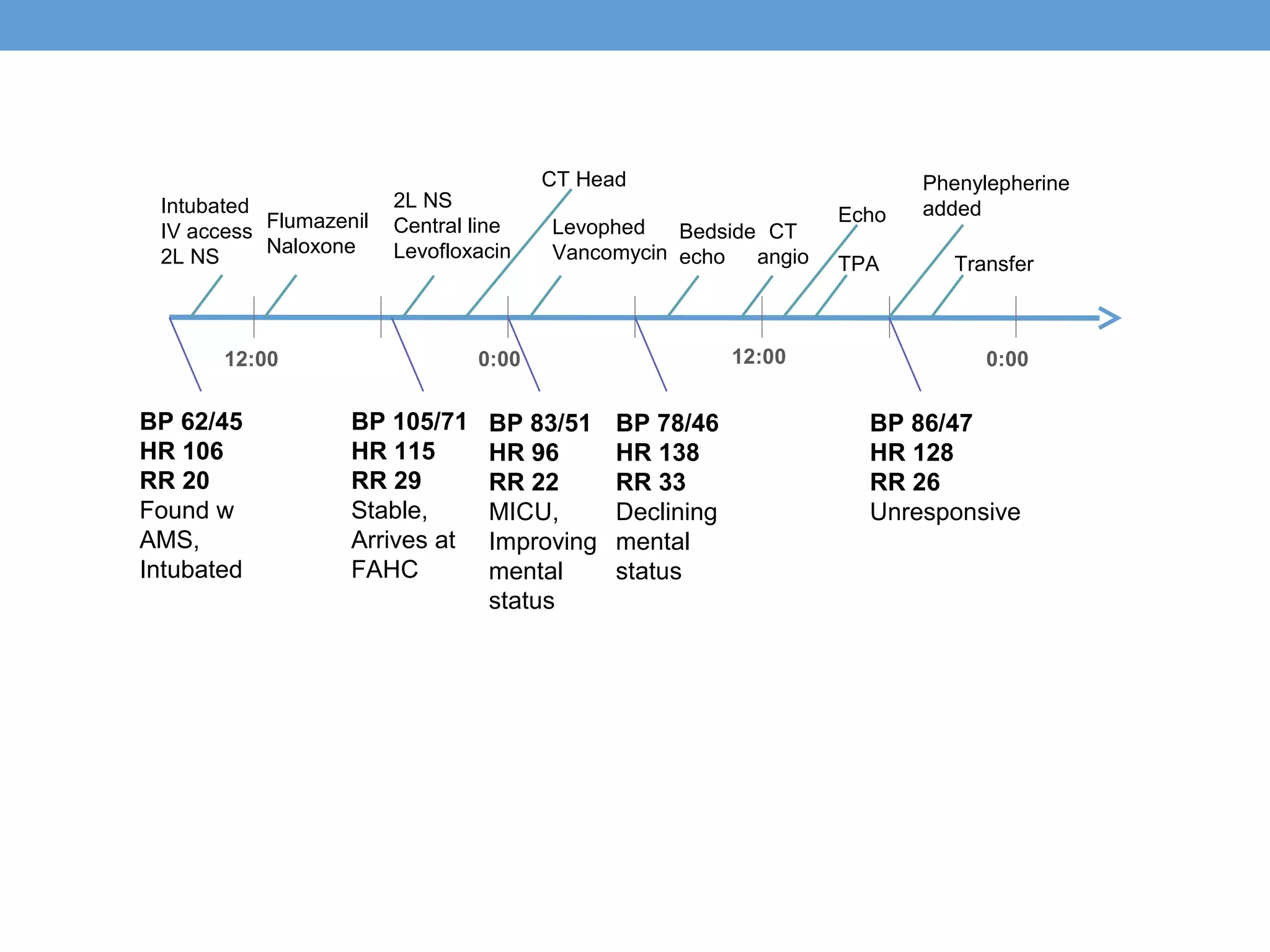
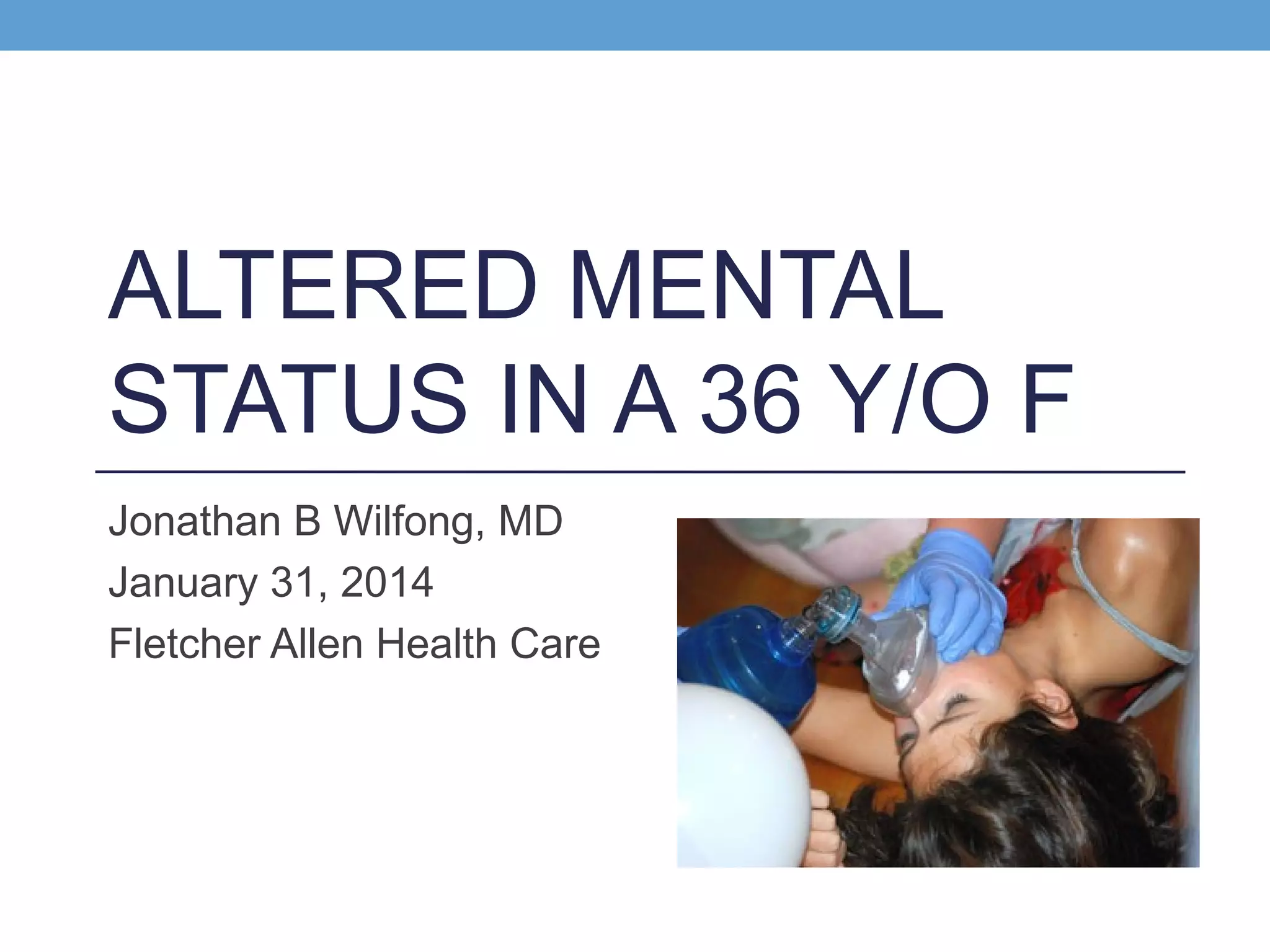
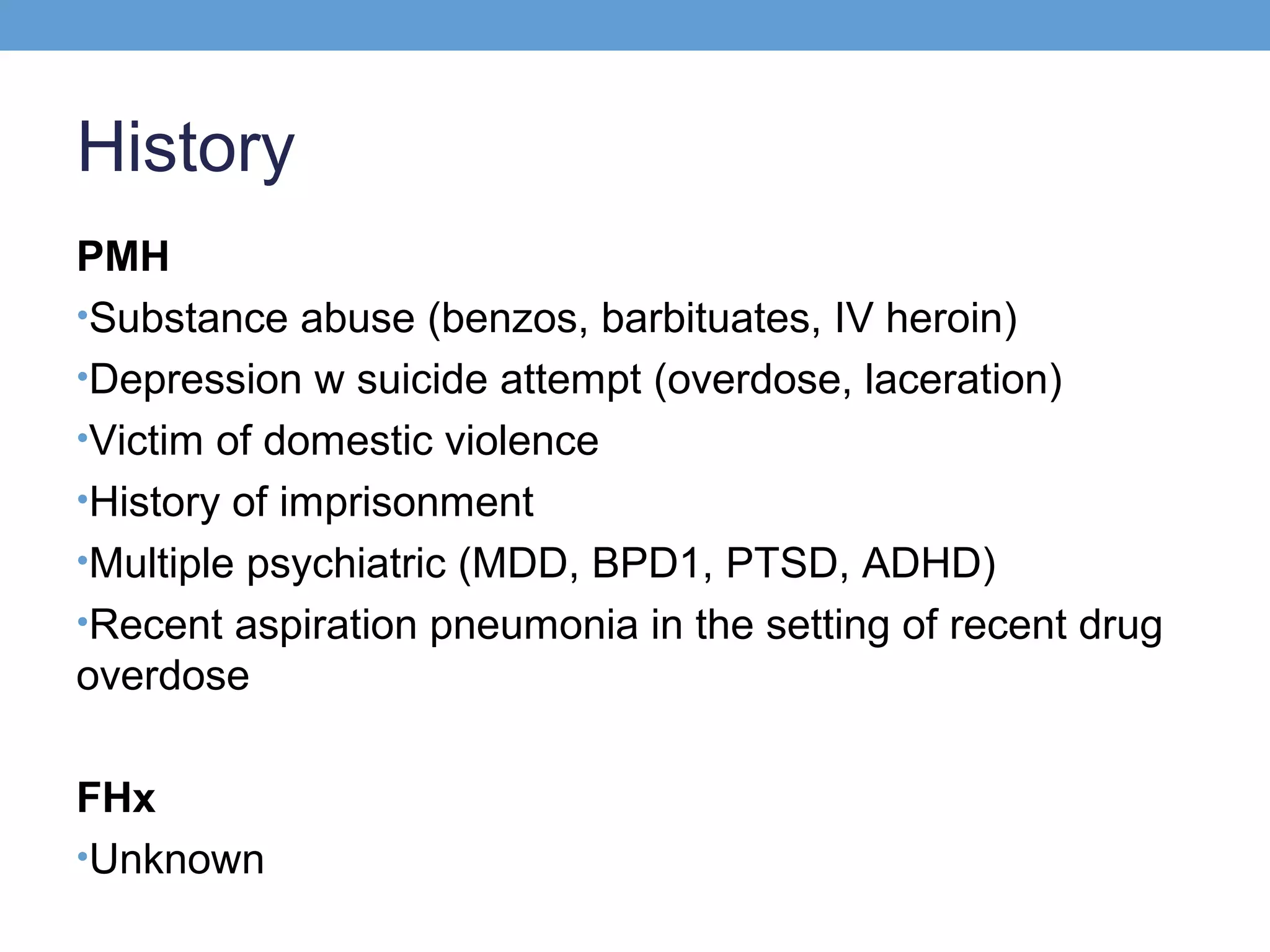
In the field [AM, Day 1]
•62/45
•106
•20
•79% SpO2 on RA
Following intubation, I/O line x2, 2L NS [18:00, Day 1]
•105/71
•115
•29
•100% SpO2 on 0.70 FiO2](https://image.slidesharecdn.com/pemassivewilfong-140131144611-phpapp01/75/Pe-massive-wilfong-6-2048.jpg)
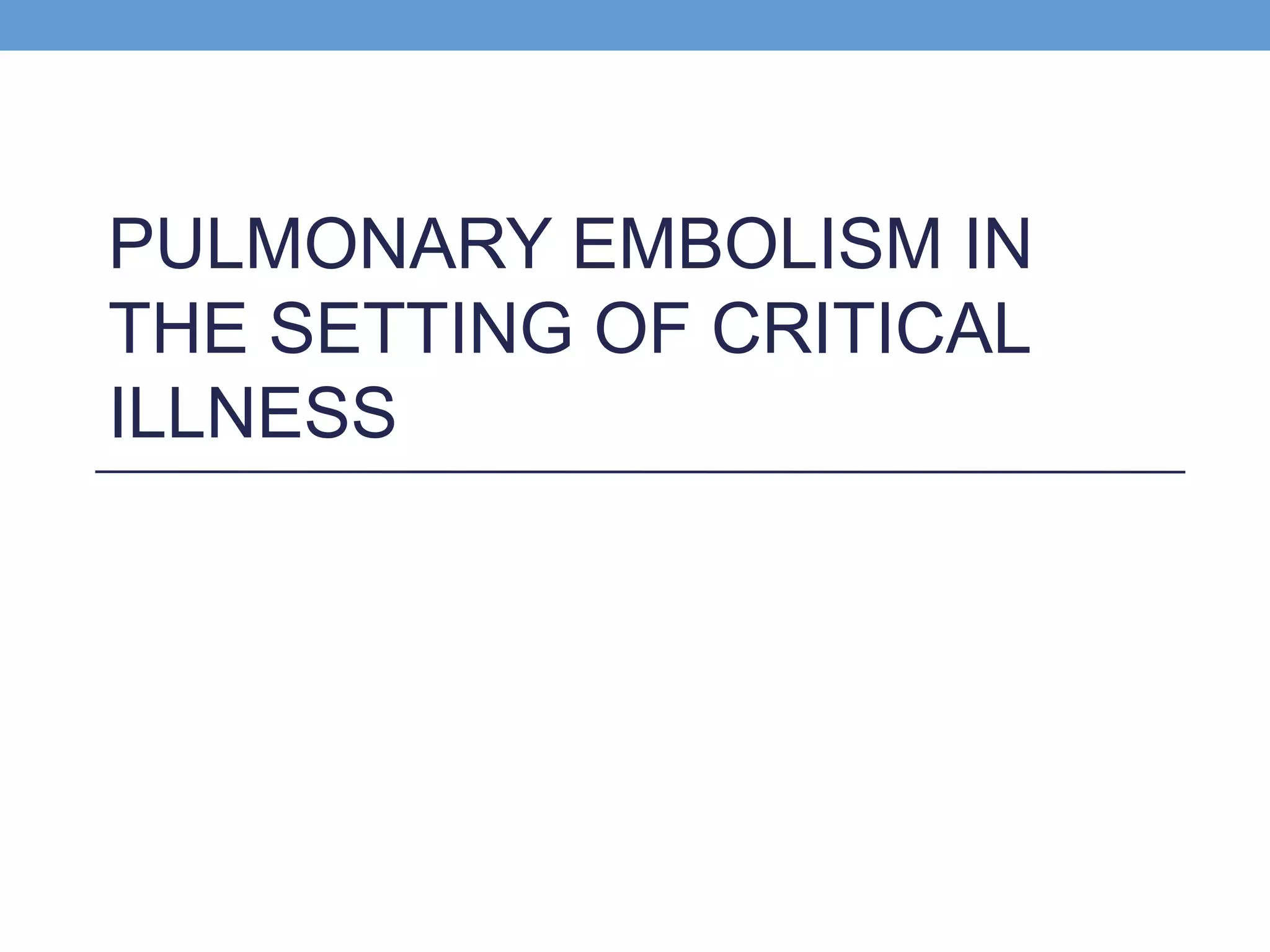
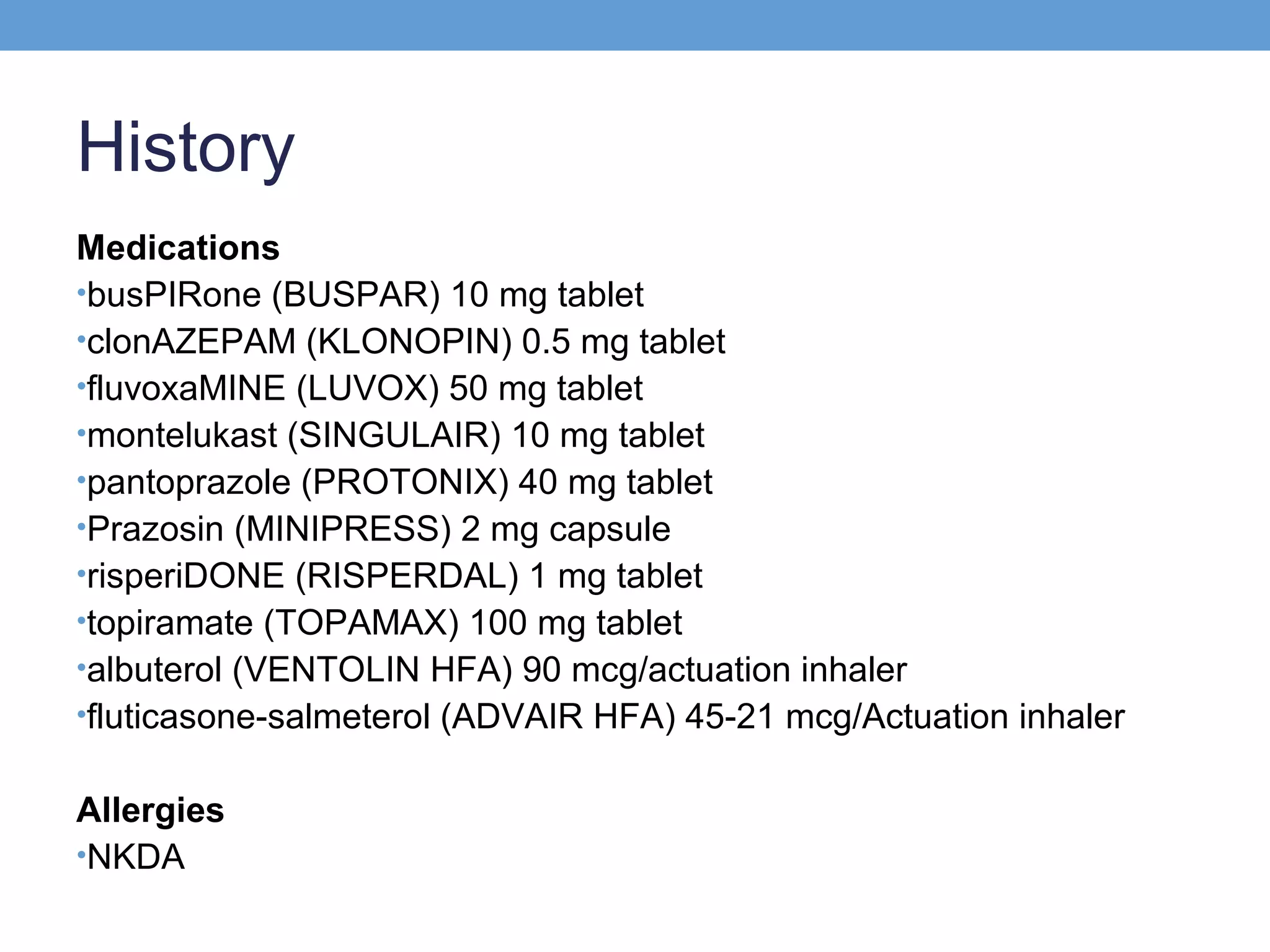
![Management
• 33.7C , 83/51, 96, 22, GCS 8, ventilated [0:00, Day 2]
• Aspiration in the setting of poly-substance use was
suspected.
• Pulm: Levofloxacin, Vanc, tapering off ventilator
• Cor: IV fluid resuscitation, serial lactate, serial EKG
• RenalL: Foley catheter, monitor UOP
• Neuro: Head CT negative, Serial neuro exams
• GI: NPO
• ID: Sputum, Blood, Urine Cx. Abx as above
• PPx: PPI, SQ Heparin, SCD](https://image.slidesharecdn.com/pemassivewilfong-140131144611-phpapp01/75/Pe-massive-wilfong-11-2048.jpg)
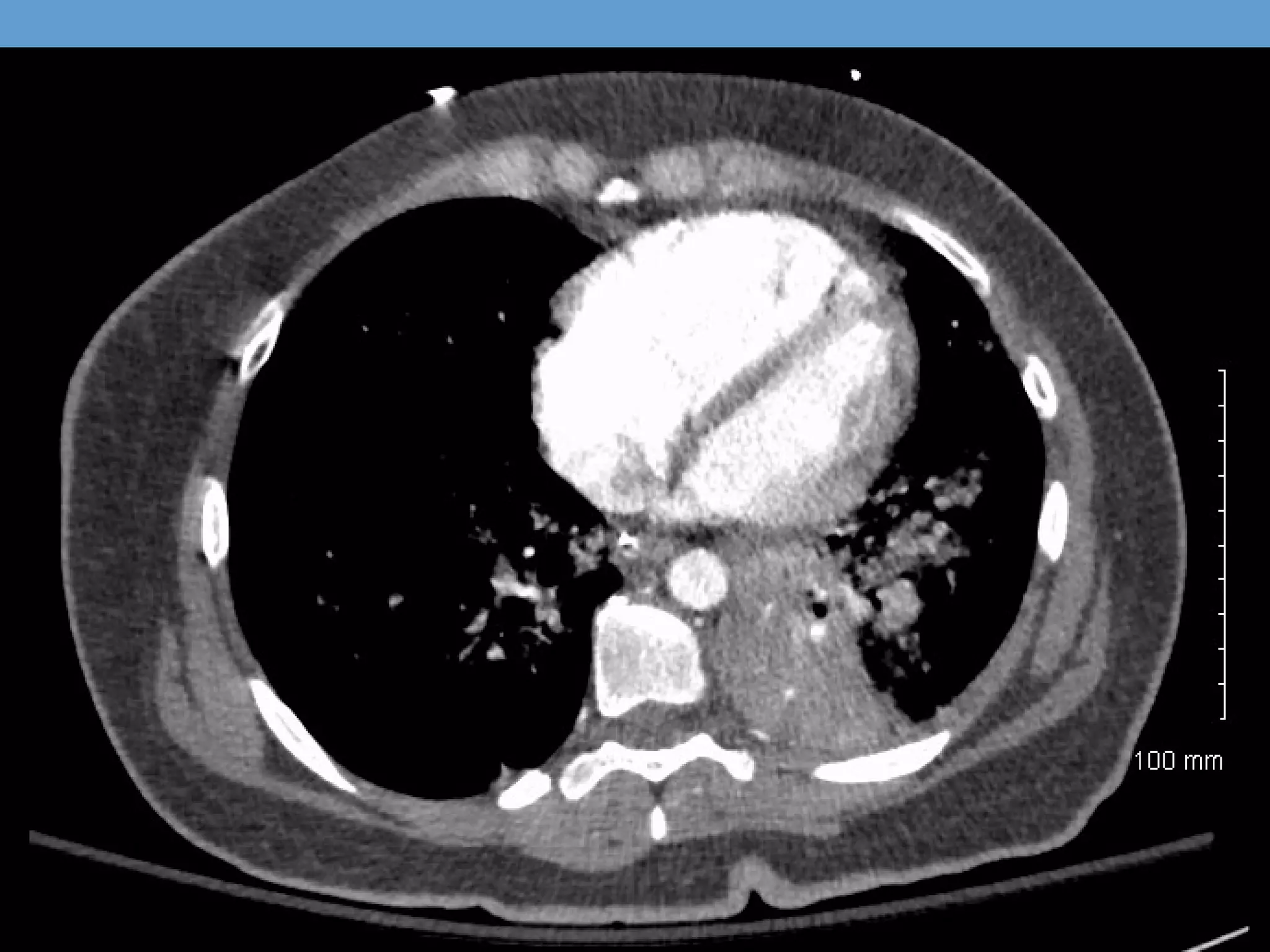
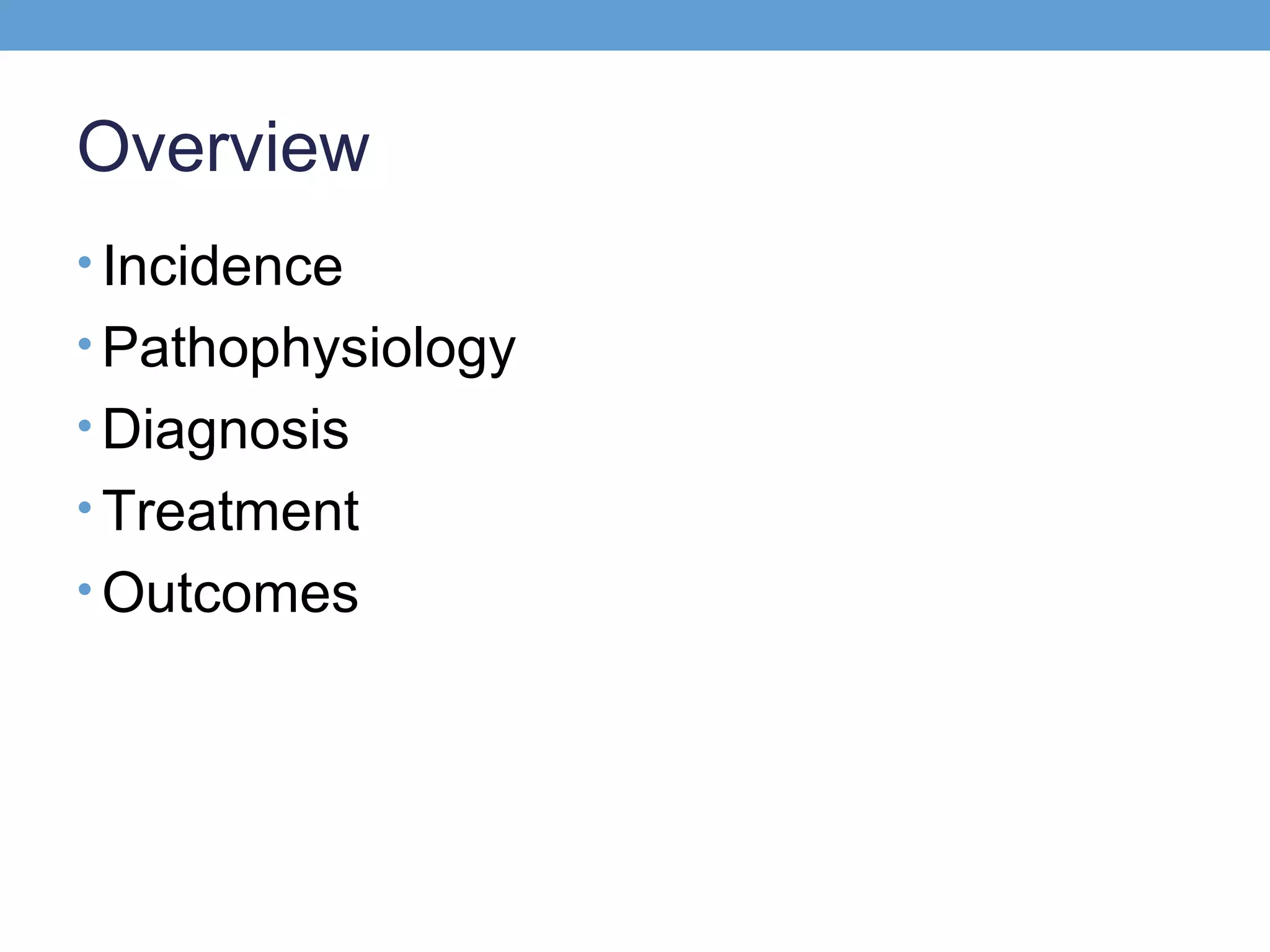
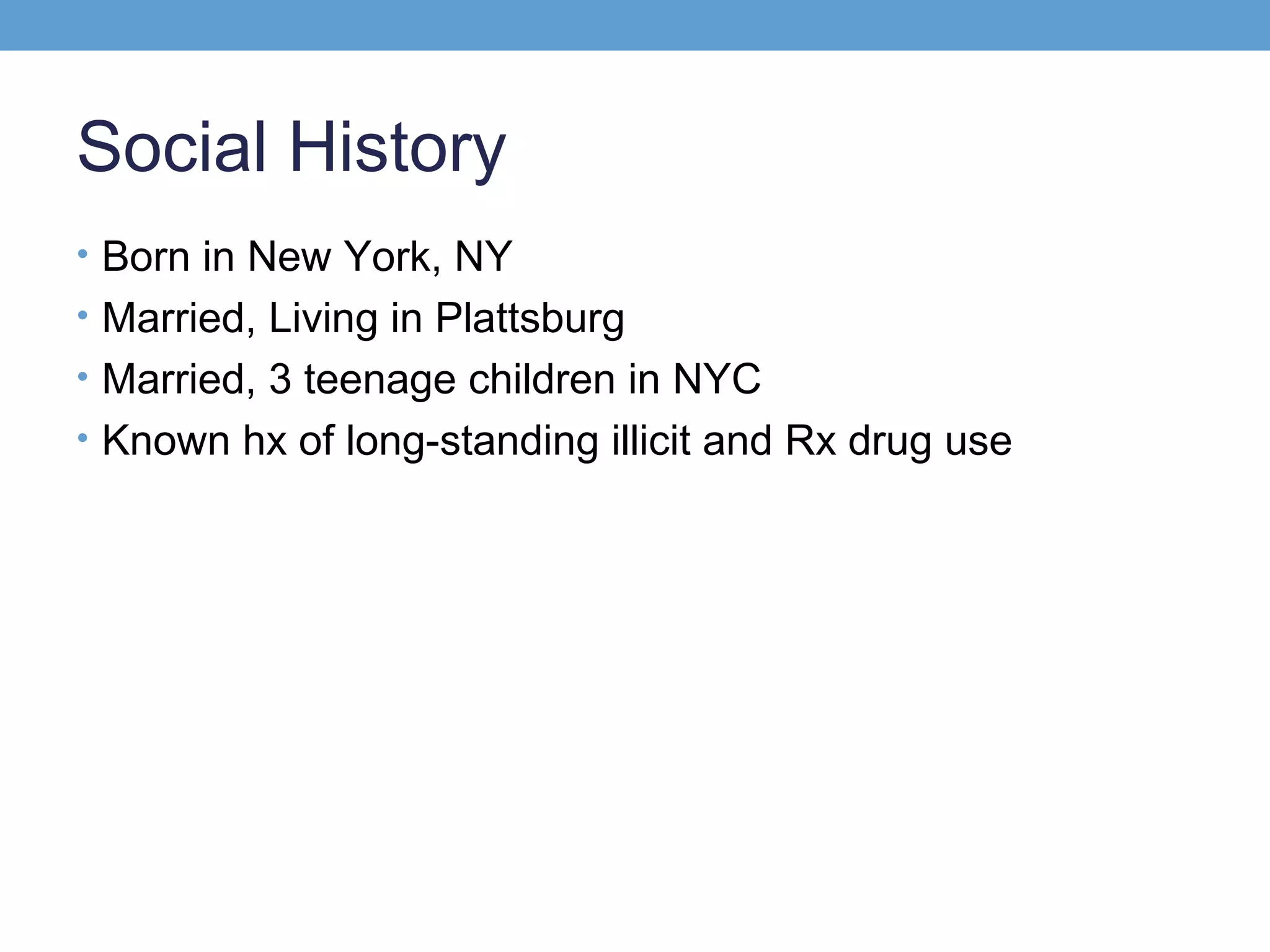
![Day of Hospitalization #2
• 7.38 / 30 / 60 / 18 on 0.55 (PaO2:FiO2 109) [05:00, Day 2]
• Improving mental status, responding to commands
but…
• Systolic pressure continued to drop despite 4L IVf
78/46, 138, 33, 98% on 0.60
• Levophederine gtt started
The patient was declining despite aggressive supportive
care.](https://image.slidesharecdn.com/pemassivewilfong-140131144611-phpapp01/75/Pe-massive-wilfong-12-2048.jpg)