- Cleft lip and palate is one of the most common birth defects, affecting approximately 1 in 1000 children. It can occur alone or as part of a genetic syndrome.
- The rates vary by ethnicity, with Asian populations having the highest rates and Black populations having the lowest. Males are more commonly affected than females.
- Clefts are repaired through surgery, with the timing varying by whether it involves the lip, soft palate, or hard palate. The goal is to close the defect and restore normal function.
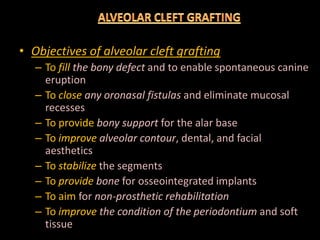
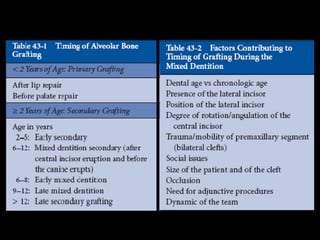
- Alveolar bone grafts are often needed to support tooth eruption and development of the midface. The optimal timing is between ages 8-12 years.