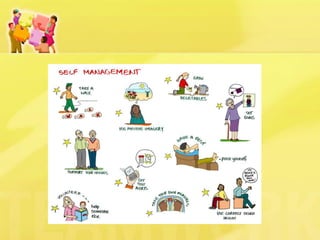
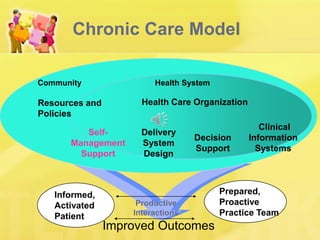
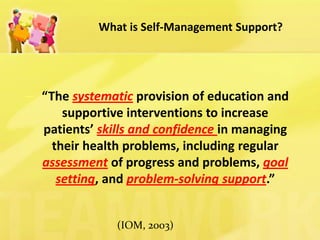
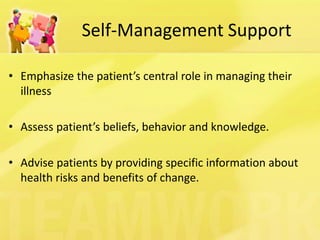
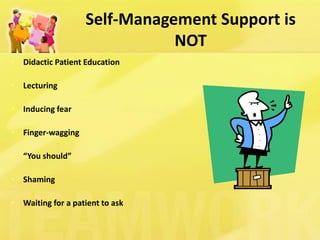
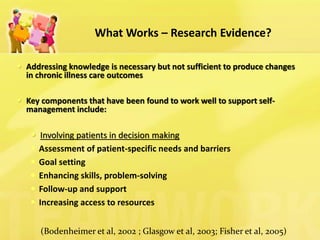
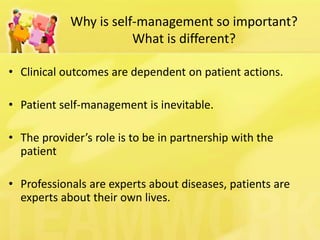
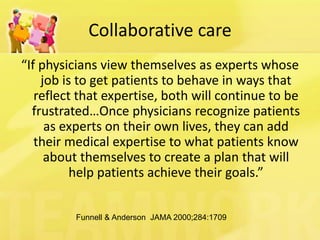
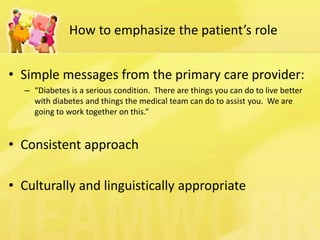
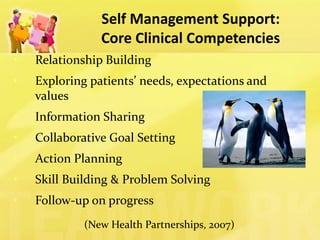
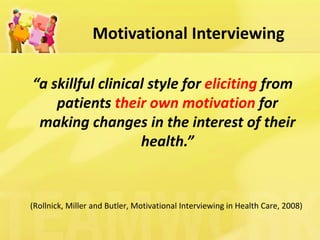
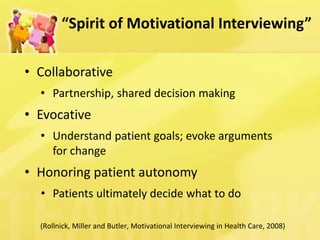
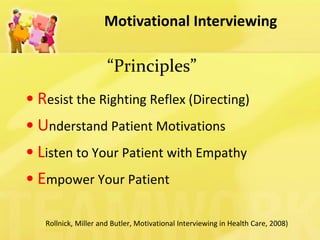
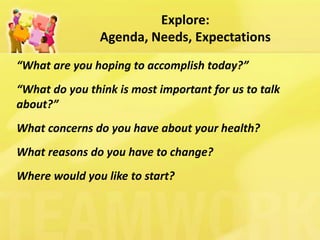
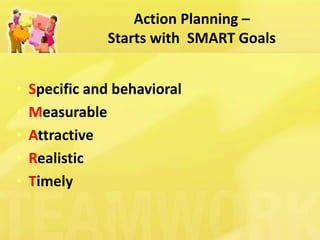
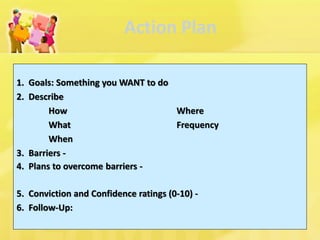
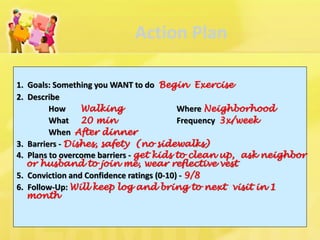
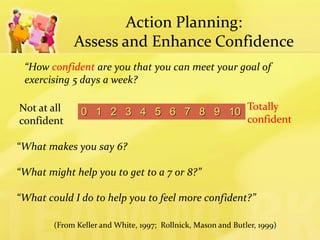
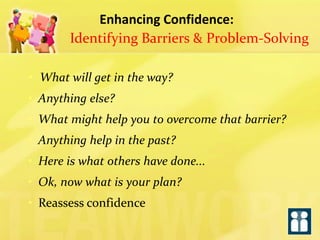
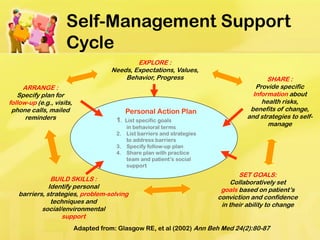
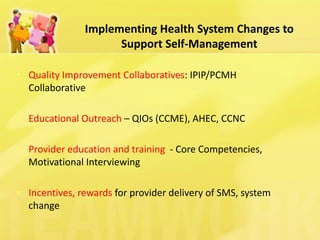
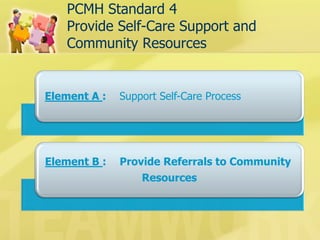
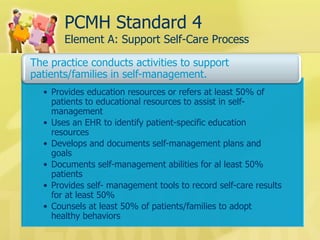
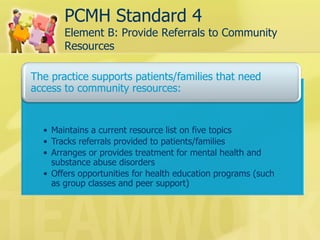
This document discusses patient self-management support, which involves helping patients manage their chronic conditions through education, goal-setting, and developing self-management skills. It describes strategies for supporting self-management, including assessing patient needs and barriers, collaborative goal-setting, enhancing problem-solving skills, and arranging follow-up care. The document also outlines how practices can meet NCQA standards for self-management support and provides resources for implementing self-management programs.