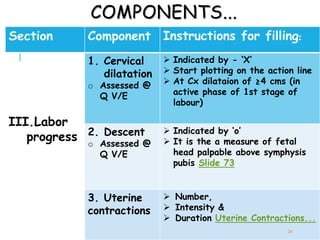
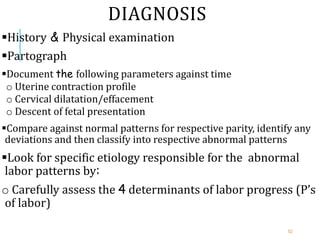
The document discusses labor monitoring using a partograph. It outlines the components and steps for documenting findings on the partograph, including monitoring cervical dilation, descent of the fetal head, uterine contractions, fetal heart rate, and maternal vital signs. Abnormal labor patterns that cross the alert or action lines on the partograph indicate slow progress and need for further evaluation or referral. The partograph is an important tool for early detection of abnormalities to prevent prolonged labor and improve maternal and neonatal outcomes.