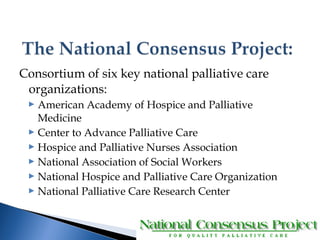
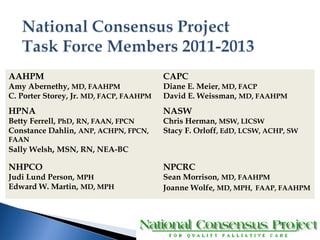
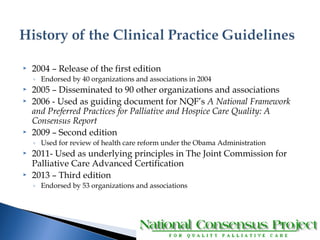
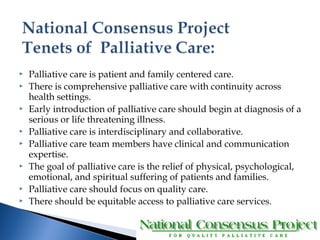
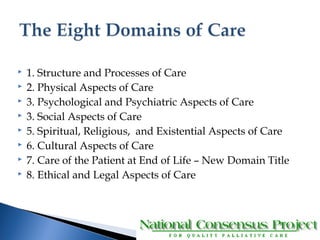
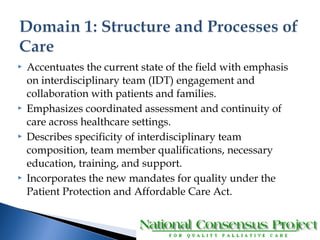
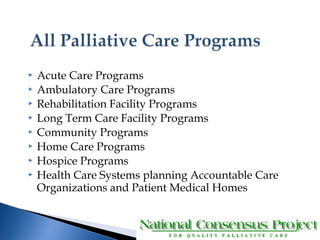
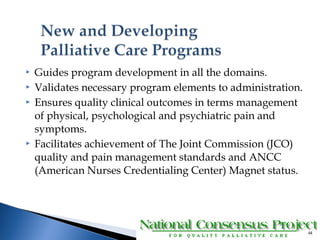
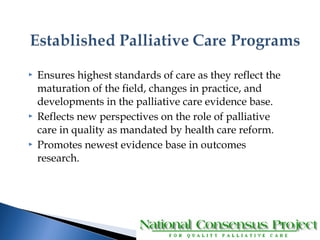
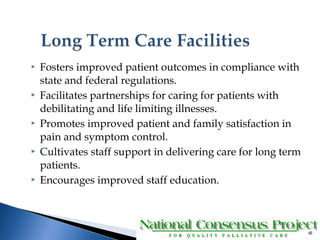
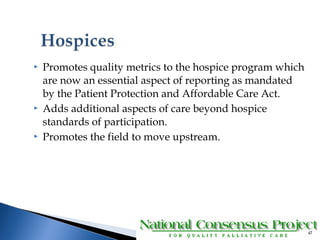
The document summarizes the 3rd edition of the National Consensus Project for Quality Palliative Care Clinical Practice Guidelines. It was created by a consortium of six palliative care organizations to improve palliative care quality in the US. The guidelines provide recommendations for interdisciplinary palliative care delivery across various clinical domains and settings. The 3rd edition features expanded recommendations regarding palliative care delivery requirements and quality standards based on recent healthcare reforms and evidence.