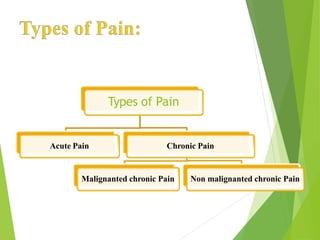
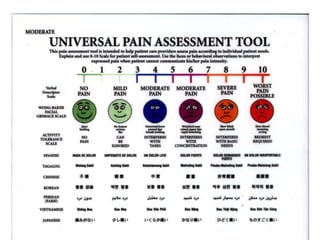
1. Acute pain is short-term pain lasting less than 6 months resulting from injury or illness, while chronic pain lasts longer than 6 months and can be malignant (cancer-related) or non-malignant.
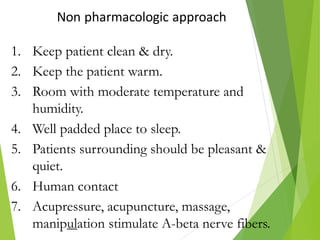
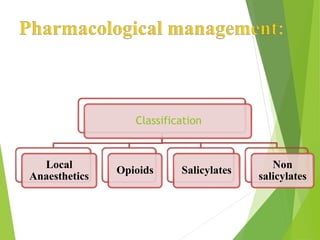
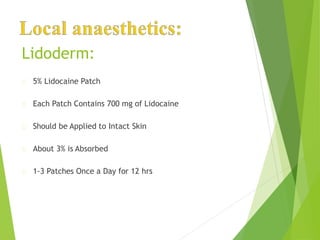
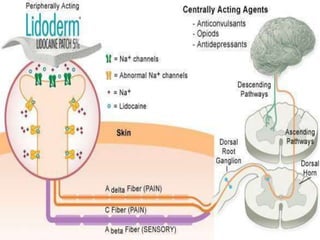
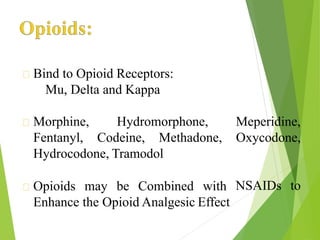
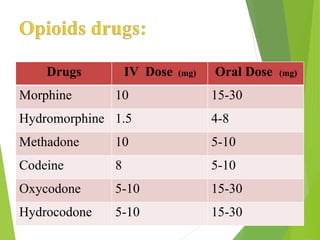
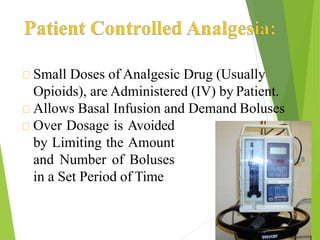
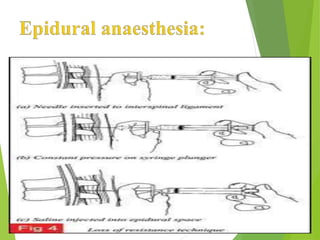
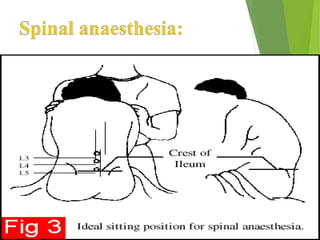
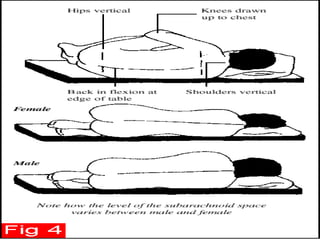
2. Pain management aims to relieve pain and associated physiological changes through pharmacological methods like opioids, NSAIDs, and local anesthetics or interventional methods like epidural anesthesia.
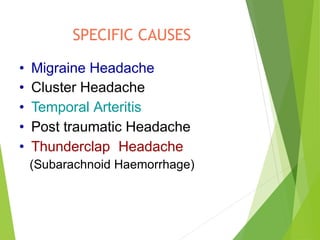
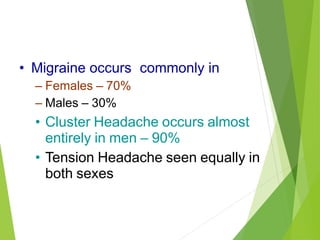
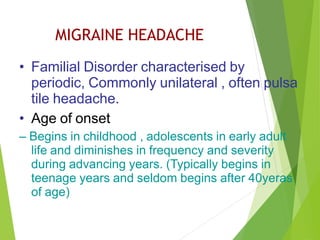
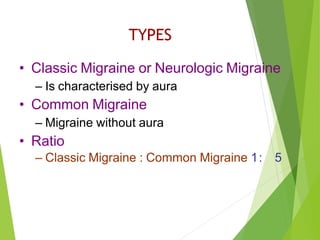
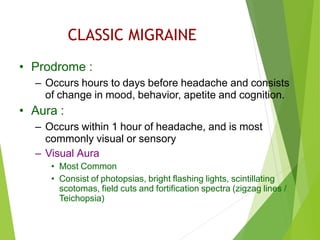
3. Migraine headaches commonly affect females and present with prodromal symptoms before an aura of visual disturbances and severe headache, while tension headaches equally affect both sexes with constant non-pulsatile pain.