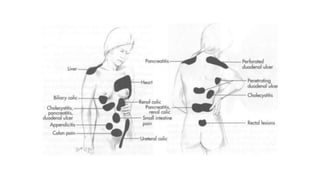
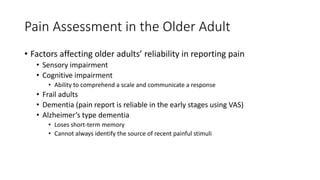
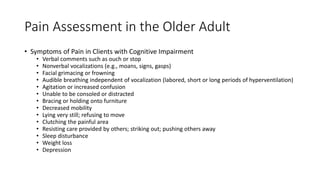
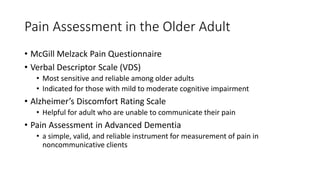
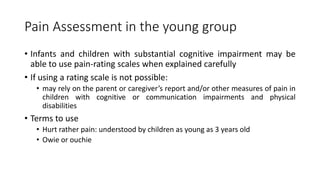
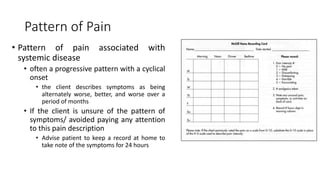
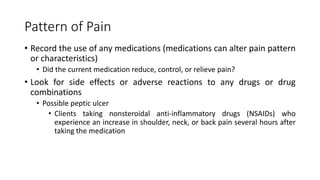
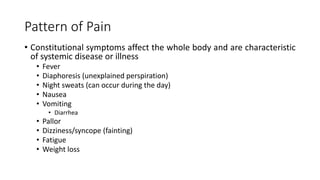
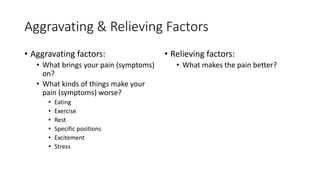
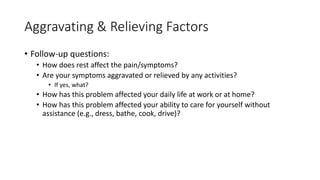
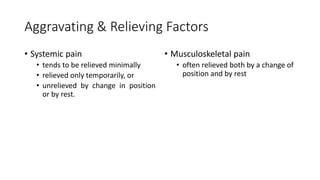
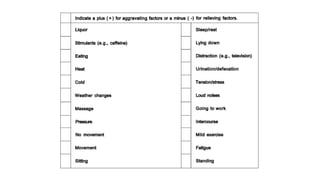
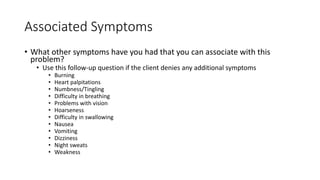
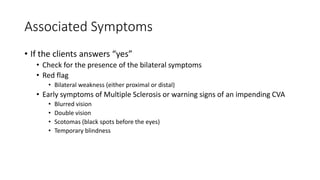
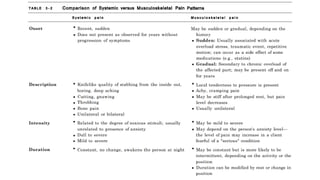
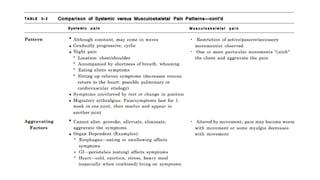
The document outlines mechanisms and assessment techniques for understanding and evaluating pain, particularly viscerogenic and referred pain associated with various body systems. It addresses the challenges in pain perception and reporting, especially in older adults and young children, highlighting specific assessment tools suitable for different demographics. Additionally, it provides guidance on identifying pain characteristics, patterns, aggravating and relieving factors, and the significance of associated symptoms in clinical settings.