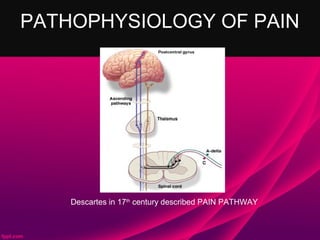
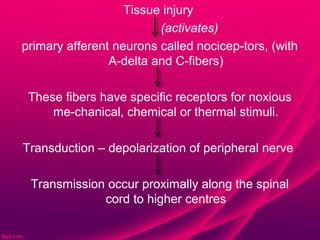
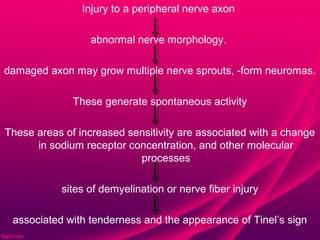
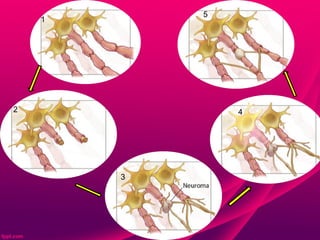
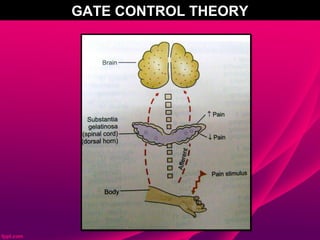
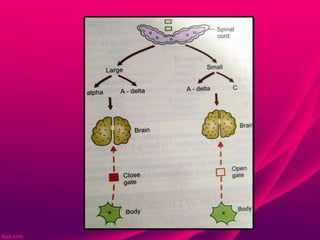
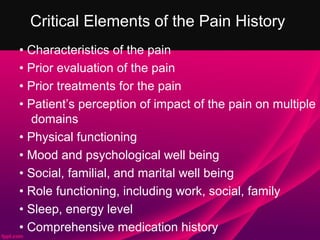
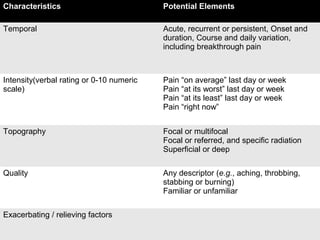
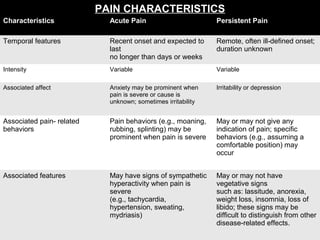
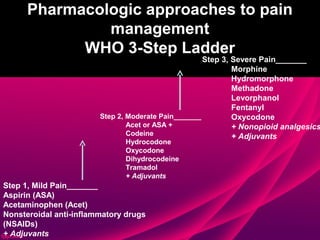
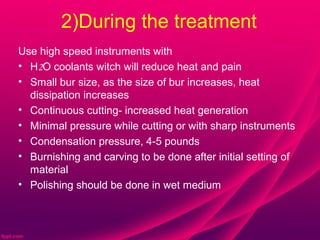
The document provides an overview of pain, including definitions, types, pathophysiology, assessment, and management. It defines pain, outlines the three levels of pain, and describes the major types. It discusses the gate control theory of pain and the pathways involved in nociceptive, neuropathic, and psychogenic pain. The document emphasizes the importance of a thorough pain assessment and outlines the critical elements to evaluate. It also summarizes different pharmacological and non-pharmacological approaches to pain management, including the WHO analgesic ladder and various local anesthesia techniques for controlling dental pain.