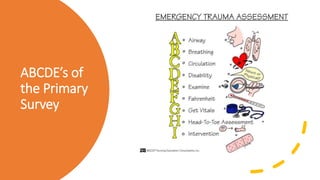
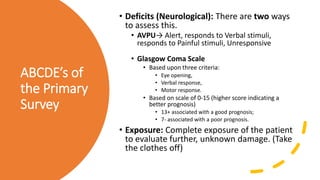
This document discusses trauma and traumatic conditions that are often highlighted during orthopedic surgery interviews. It provides guidance on evaluating trauma patients, including performing a trauma-specific workup that assesses the ABCDEs of the primary survey (airway, breathing, circulation, deficits, exposure), tetanus status, and NPO status. Key traumatic emergencies discussed include open fractures, compartment syndrome, necrotizing fasciitis, gas gangrene, and neurovascular compromise. Classification systems for open fractures and wound characterization are presented. The diagnosis and treatment of compartment syndrome is explained. The clinical presentation, imaging, and blood culture characteristics of gas gangrene are outlined.

![NPO status
• All trauma patients are potential surgical
candidates, so get this information for the weenie
anesthesiologists (Always remember that lunch is
for doctors, not for surgeons; while coffee breaks
and crossword puzzles are for anesthesiologists).
• Traditional guidelines recommend:
• Nothing by mouth after midnight the night before
elective surgery.
• Nothing by mouth within 6-8 hours of any type of
surgery.
• These strict guidelines are in the process of
changing however, particularly with regard to
allowing the ingestion of small amounts of clear
liquids up to the time of surgery. If interested,
please read:
[Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane
Database Syst Rev. 2003; (4): CD004423.]
[Murphy GS, et al. The effect of a new NPO policy on operating room utilization. J Clin Anesth. 2000 Feb;
12(1): 48-51.]](https://image.slidesharecdn.com/ajmtrauma-5emergencies-200517214113/85/AJM-Sheet-5-Podiatric-Emergencies-10-320.jpg)

![Gustilo-Anderson Classification of Open Fractures [Gustilo RB, Anderson JT. Prevention of
infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses.
JBJS-Am. 1976; 58(4): 453-8.]](https://image.slidesharecdn.com/ajmtrauma-5emergencies-200517214113/85/AJM-Sheet-5-Podiatric-Emergencies-15-320.jpg)

![Mangled
Extremity Severity
Score (MESS)
based on 4
criteria (score
points)
• * A (score) of 7+ = an increased likelihood of
amputation.
• * (Score) doubled for ischemia > 6 hours
• * Based on a (score) from 1-11 with a higher score
leading to an increased incidence of amputation.
• Gustilo-Anderson Classification of Open Fractures [Gustilo RB, Anderson
JT. Prevention of infection in the treatment of one thousand and twenty-
five open fractures of long bones: retrospective and prospective analyses.
JBJS-Am. 1976; 58(4): 453-8.]
• Review Paper for IIIa-IIIb sepsis rates: GustiloRB; MerkowRL; Templeman.
Current Concepts review. The management of open fractures. J Bone Joint
Surg[Am], 72:299-304, 1990 Feb
• Amputation Rates from: Gustilo1987 paper [Helfet DL, et al. Limb salvage
versus amputation. Preliminary results of the Mangled Extremity Severity
Score. CORR 1990; 256: 80-6.]
• [Bosse MJ, et al. A prospective evaluation of the clinical utility of the
lower-extremity injury-severity scores. JBJS-Am 2001; 83(1): 3-14.]](https://image.slidesharecdn.com/ajmtrauma-5emergencies-200517214113/85/AJM-Sheet-5-Podiatric-Emergencies-18-320.jpg)
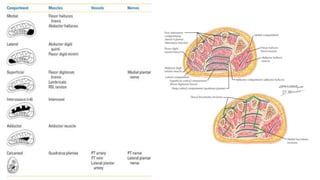
![How many
compartments
are there?
The foot has anywhere from 3-11 compartments depending on
who you read:
1. Intermetatarsal Compartments X 4: Contains the interossei
muscles
2. Medial Compartment: Abductor Hallucis
3. Lateral Compartment: Abductor digiti minimi
4. Superficial Central Compartment: FDB
5. Deep Central Compartment: Adductor Hallucis
6. Calcaneal Compartment: Quadratus Plantae
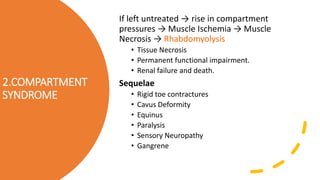
• Compartment Syndrome
• First described by Volkmann. Myerson has good articles/chapters on this topic.
• [Perry MD, Manoli A. Foot compartment syndrome. Orthop Clin North Am. 2001 Jan; 32(1):
103-11.]
• [Myerson M, Manoli A. Compartment syndromes of the foot after calcaneal fractures. Clin
Orthop Relat Res. 1993 May: 142-50.]
• Results when interstitial pressure exceedscapillary hydrostatic pressure, so the
microcirculation shuts down.
• The foot has anywhere from 3-11 compartments depending on who you read:
1. Intermetatarsal Compartments X 4: Contains the interossei muscles
2. Medial Compartment: Abductor Hallucis
3. Lateral Compartment: Abductor digiti minimi
4. Superficial Central Compartment: FDB
5. Deep Central Compartment: Adductor Hallucis
6. Calcaneal Compartment: Quadratus Plantae and lateral plantar artery
7. Dorsal Compartment: EHB and EDB](https://image.slidesharecdn.com/ajmtrauma-5emergencies-200517214113/85/AJM-Sheet-5-Podiatric-Emergencies-23-320.jpg)

![Complications
• Permanent loss of function with structural
deformity (Volkmann contractures),
myoneural necrosis, sensory loss, chronic
pain
[Perry MD, Manoli A. Foot compartment syndrome. Orthop Clin North Am. 2001 Jan; 32(1):
103-11.]
[Myerson M, Manoli A. Compartment syndromes of the foot after calcaneal fractures. Clin
Orthop Relat Res. 1993 May: 142-50.]](https://image.slidesharecdn.com/ajmtrauma-5emergencies-200517214113/85/AJM-Sheet-5-Podiatric-Emergencies-28-320.jpg)

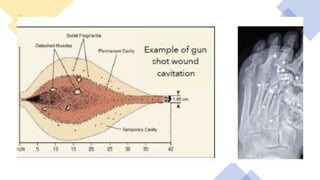
![Gun Shot
Wounds
• High velocity GSWs are characterized by
speeds >2500 ft/s. This is significant because
high velocity GSWs have a tendency to yaw
and tumble leading to increased cavitation.
• Cavitation: Large wound is created under a
situation of negative pressure. This
• Negative pressure “sucks” outside
contaminants into the wound.
(Ordog classification for gunshot wounds)
[Holmes GB. Gunshot wounds of the foot.
CORR. 2003 Mar; (408): 86-91.]](https://image.slidesharecdn.com/ajmtrauma-5emergencies-200517214113/85/AJM-Sheet-5-Podiatric-Emergencies-43-320.jpg)

![Resnick
Classification
• I. Superficial/cutaneous: usually visible
without signs of infection.
• II. Subcutaneous or articular without signs of
infection.
• IIIA. Subcutaneous or articular with signs of
infection.
• IIIB. Bone penetration without signs of
infection.
• IV. Bone penetration with known
osteomyelitis.
[Resnick CD. Puncture wounds: therapeutic considerations and a
new classification. J Foot Surg. 1990 Mar-Apr; 29(2): 147-53.]](https://image.slidesharecdn.com/ajmtrauma-5emergencies-200517214113/85/AJM-Sheet-5-Podiatric-Emergencies-46-320.jpg)
![Patzakis
Classification
• Zone 1: Toes to met head
• (50% incidence of osteomyelitis)
• Zone 2: Midfoot
• (17% incidence of osteomyelitis)
• Zone 3: Calcaneus
• (33% incidence of osteomyelitis)
[Patzakis MJ. Wound site as a predictor of complications following deep
nail punctures of the foot. West J Med. 1989 May; 150(5): 545-7.]](https://image.slidesharecdn.com/ajmtrauma-5emergencies-200517214113/85/AJM-Sheet-5-Podiatric-Emergencies-47-320.jpg)