Major Neurotransmitters and Their Functions
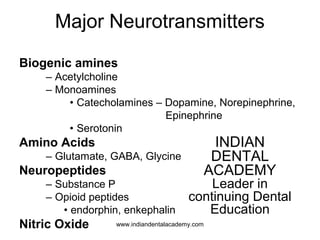
- 1. Major Neurotransmitters Biogenic amines – Acetylcholine – Monoamines • Catecholamines – Dopamine, Norepinephrine, Epinephrine • Serotonin Amino Acids – Glutamate, GABA, Glycine Neuropeptides – Substance P – Opioid peptides • endorphin, enkephalin Nitric Oxide INDIAN DENTAL ACADEMY Leader in continuing Dental Education www.indiandentalacademy.com
- 2. Neurotransmitters are divided into 2 types- • Small rapid acting molecules –Acetylcholine, Norepinephrine, Glutamate, Aspartate, Serotonin(excitatory) - GABA, Glycine, dopamine(Inhibitory) • Larger slower acting molecules- Substance P, Endorphins www.indiandentalacademy.com
- 3. Acetylcholine Produced by- In Brain -Motor cortex, the basal ganglion In PNS – Motor neurons – Parasympathetic • Both pre- and postganglionic neurons – Sympathetic • pre-ganglionic neurons • some post-ganglionic neurons that innervate sweat glands and blood vessels www.indiandentalacademy.com
- 4. • Acetylcholine is a very widely distributed excitatory neurotransmitter that triggers muscle contraction and stimulates the excretion of certain hormones. In the central nervous system, it is involved in wakefulness, attentiveness, anger, aggression, sexuality, and thirst, among other things. • Alzheimer’s disease is associated with a lack of acetylcholine in certain regions of the brain www.indiandentalacademy.com
- 5. Norepinephrine • Norepinephrine is a neurotransmitter that is important for attentiveness, emotions, sleeping, dreaming, and learning. • Norepinephrine is also released as a hormone into the blood, where it causes blood vessels to contract and heart rate to increase. • Norepinephrine plays a role in mood disorders such as manic depression. www.indiandentalacademy.com
- 7. Glutamate • Glutamate is a major excitatory neurotransmitter secreted by presynaptic terminals in many sensory pathways as well as in many areas of the cortex and is associated with learning and memory. It is also thought to be associated with Alzheimer’s disease, whose first symptoms include memory malfunctions. Aspartate It is secreted by presynaptic terminals in many sensory pathways in the dorsal horn. It is thought to always cause excitation www.indiandentalacademy.com
- 8. • Serotonin contributes to various functions, such as regulating body temperature, sleep, mood, appetite, and pain. Depression, suicide, impulsive behaviour, and aggressiveness all appear to involve certain imbalances in serotonin. • It is released by blood platelets • In CNS is synthesized from L-Tryptophan and released from nucleus magnus when stimulated from sensory input. • Peripherally it is an algogenic agent • In CNS it is an important chemical in the endogenous antinoniceptive mechanism. www.indiandentalacademy.com
- 10. • Dopamine is an inhibitory neurotransmitter involved in controlling movement and posture. It also modulates mood and plays a central role in positive reinforcement and dependency. • The loss of dopamine in certain parts of the brain causes the muscle rigidity typical of Parkinson’s disease. www.indiandentalacademy.com
- 12. Glycine It is secreted by many areas of spinal cord and likely to be secreted in the trigeminal spinal nucleus.It is probably always an inhibitory transmitter. HISTAMINE Vasoactive amine derived from histadine Also a vasodilator and increases small vessel permeability Causes contraction of smooth muscles in the lungs www.indiandentalacademy.com
- 13. • GABA (gamma-aminobutyric acid) is an inhibitory neurotransmitter that is secreted by the neurons in the spinal cord,cerebellum,basal ganglia, and parts of the cortex. • GABA contributes to motor control.It also regulates anxiety. • Some drugs that increase the level of GABA in the brain are used to treat epilepsy and to calm the trembling of people suffering from Huntington’s disease. www.indiandentalacademy.com
- 14. Substance P • Belongs to family of proteins called tachykinins • 11 amino acids polypeptide • Found in primary afferent nerve endings (C fibres),substantia gelatinosa of cord, substantia nigra • Roles in– pain transmission / inflammation, nausea,mood/depression, migraine www.indiandentalacademy.com
- 15. ENDORPHINS • Endorphins can be found in the pitutary gland, in other parts of the brain, or distributed throughout the nervous system. • Stress and pain are the two most common factors leading to the release of endorphins. Endorphins interact with the opiate receptors in the brain to reduce our perception of pain and act similarly to drugs such as morphine and codeine. In contrast to the opiate drugs, however, activation of the opiate receptors by the body's endorphins does not lead to addiction or dependence. • In addition to decreased feelings of pain, secretion of endorphins leads to feelings of euphoria, modulation of appetite, release of sex hormones, and enhancement of the immune response. With high endorphin levels, we feel less pain and fewer negative effects of stress www.indiandentalacademy.com
- 16. Orofacial Pain-II Guided by Dr Shirish S. Degwekar Presented by Sangeeta Malik www.indiandentalacademy.com
- 17. Contents-Part-I The Nature of Pain • Definition • Neural anatomy of orofacial pain • Neurophysiology of orofacial pain • Central processing and Psychology of pain Clinical considerations of pain • Measurement of Pain and Disability • History of Orofacial pain • Orofacial Pain Clinical examination • Establishing the pain category • Confirmation of clinical diagnosis Classification of orofacial painwww.indiandentalacademy.com
- 18. PART-II • Clinical pain Syndromes • General Considerations in Managing Orofacial pains. www.indiandentalacademy.com
- 19. Classification of orofacial pain www.indiandentalacademy.com
- 20. • Somatic Pain Noxious impulses being received and transmitted by normal components of the sensory nervous system.(normal neural structures –abnormal somatic structures) • Neuropathic Pain Noxious impulses originating from an abnormality in neural structures.(abnormal neural structures - normal somatic structures) www.indiandentalacademy.com
- 22. Superficial Somatic Pain 1. The pain has a bright, stimulating quality. 2. Subjective localization of the pain is excellent and anatomically accurate. 3. The site of pain identifies the correct location of its source. 4. Response to provocation at the site of pain is faithful in incidence, intensity, and location. 5. The application of a topical anesthetic at the site of pain temporarily arrests it. www.indiandentalacademy.com
- 23. Superficial somatic • Cutaneous Pain • Mucogingival Pain www.indiandentalacademy.com
- 24. Mucogingival pains of the mouth Etiology- • Trauma • Allergic • Local infections • Systemic conditions • Or may present as burning mouth syndrome www.indiandentalacademy.com
- 25. • Since the pain of Mucogingival origin is an expression of primary hyperalgesia of the tissue that hurt, application of a topical anaesthetic to those tissues arrests the pain due to action of the medication on the receptors and pain fibres in the mucogingival tissues. www.indiandentalacademy.com
- 26. Burning Mouth Syndrome (Glossodynia) (Mucogingival pain) Burning sensations accompany many inflammatory or Ulcerative diseases of the oral mucosa, but the term “burning mouth syndrome” (BMS) is reserved for describing oral burning that has no detectable cause. The burning symptoms in patients with BMS do not follow anatomic pathways, there are no mucosal lesions or known neurologic disorders to explain the symptoms,and there are no characteristic laboratory abnormalities. www.indiandentalacademy.com
- 27. ETIOLOGY • Hormonal • Allergic disorders • Salivary gland hypofunction • Chronic low-grade trauma • And psychiatric abnormalities. www.indiandentalacademy.com
- 28. • Dysgeusia (particularly an abnormally bitter taste) has been reported by 60% of BMS patients.This association has led to a concept that BMS may be a defect in sensory peripheral neural mechanisms. www.indiandentalacademy.com
- 29. Clinical Features • Women experience symptoms of BMS seven times more frequently than men. • 10 to 15% of postmenopausal women are found to have a history of oral burning sensations, and these symptoms are most prevalent 3 to 12 years after menopause. • Tongue is the most common site of involvement, but the lips and palate are also frequently involved. www.indiandentalacademy.com
- 30. • The burning can be either intermittent or constant, but eating, drinking, or placing candy or chewing gum in the mouth characteristically relieves the symptoms. • This contrasts with the increased oral burning noted during eating that occurs in patients with lesions or neuralgias affecting the oral mucosa. • Patients presenting with BMS are often apprehensive and admit to being generally anxious or “high-strung.” www.indiandentalacademy.com
- 31. Treatment of burning mouth syndrome • Eliminating the possibility of detectable lesions or underlying medical disorders • Counseling and reassurance may be adequate management for individuals with mild burning sensations, but patients with symptoms that are more severe often require drug therapy. • The drug therapies that have been found to be the most helpful are low doses of TCAs, such as amitriptyline and doxepin, or clonazepam (a benzodiazepine Derivative). www.indiandentalacademy.com
- 32. Differential Diagnosis Of Superficial Somatic Cutaneous or Mucogingival Pain • 1)Heterotopic pain • 2)Paroxysmal Neuralgia • 3)Deafferentation Pain • 4)Traumatic neuroma • 5)Neuritis • 6)Herpes Zoster www.indiandentalacademy.com
- 33. Therapeutic options of Superficial Somatic Cutaneous or Mucogingival Pain • Analgesics for palliative relief • Cause related therapy -Elimination of all oral irritants -Restriction of oral functions within reasonable limits -Antibiotics and Antimicrobials, topical and systemic -Antivirals -For Xerostomia-Paraffin or gum to stimulate saliva,saliva substitutes www.indiandentalacademy.com
- 34. • Pharmacological therapy -Topical anaesthetic -Analgesic Balm (cutaneous pain) -antiinflammatory • Medical consultations www.indiandentalacademy.com
- 35. Deep Somatic Pain 1.The pain has a dull, depressing quality. 2. Subjective localization of the pain is variable and somewhat diffuse. 3. The site of pain may or may not identify the correct location of its true source. 4. Response to provocation at the site of pain is fairly faithful in incidence and intensity but not in location. 5. Accompanying secondary central excitatory effects are frequently displayed.www.indiandentalacademy.com
- 36. There are two distinct types of deep somatic pain • Musculoskeletal pain • Visceral pain. www.indiandentalacademy.com
- 37. Musculoskeletal Pain 1.The pain is intimately related to biomechanical function. 2. The response to provocation is a gradient that is proportionate to the stimulus. Visceral Pain 1. The pain is irrelevant to biomechanical function. 2. The pain is nonresponsive to provocation until a threshold is reached. www.indiandentalacademy.com
- 38. SOMATIC PAIN DEEP PAIN Visceral pain • Neurovascular pain • Vascular pain • Pulpal pain • Visceral mucosal pain • Glandular,Occular and Auricular pain www.indiandentalacademy.com
- 39. SOMATIC PAIN DEEP PAIN Musculoskeletal pain • Periodontal pain • Soft connective tissue pain • Osseous and periosteal pain • Tempromandibular joint pain • Muscle Pain www.indiandentalacademy.com
- 40. PAINS OF DENTAL ORIGIN It may be - 1)Dental pain of pulpal origin(visceral) 2)Dental pain of Periodontal origin(musculoskeletal) www.indiandentalacademy.com
- 41. Classification of Toothaches • Pulpal disease – Reversible pulpitis (brief, stimulated pain) – Irreversible pulpitis (prolonged, stimulated or spontaneous pain) – Necrotic pulp (asymptomatic, no response to pulp testing) • Periapical disease – Acute apical periodontitis (sensitivity to percussion) – Acute apical abscess (sensitivity to percussion, swelling, pus) – Chronic apical abscess (often asymptomatic, periapical radiolucency) • Heterotopic pain – Projected pain (pain in adjacent teeth) – Referred pain (pain in teeth in opposing arch) www.indiandentalacademy.com
- 42. Characteristics of Pulpal & Periapical Pain Pulpal Pain (Deep, Somatic, Visceral) Periapical Pain (Deep, somatic, Musculoskeletal) Masticatory function (Biomechanical stimulation) Not stimulated by biting, chewing, or percussion Stimulated by biting, chewing, or percussion Localization Frequently difficult to localize specifically Usually can localize precisely Sequence Usually precedes periapical pain Usually follows pulpal pain (unless periodontitis, hyperocclusion, bruxism) www.indiandentalacademy.com
- 43. Nonodontogenic Toothaches Most toothaches will be of odontogenic origin. However, if there is no identifiable cause or source (e.g. caries) for the pain, or the history and clinical findings are inconsistent with odontogenic pain, then a nonodontogenic source should be considered. www.indiandentalacademy.com
- 44. Heterotopic Pain • Pain felt in an area other than its true site of origin (associated with deep, somatic pain). – Projected pain: perceived in the anatomic distribution of the same nerve that mediates the primary pain (painful adjacent teeth). – Referred pain: felt in an area innervated by a different nerve from the one that mediates the primary pain (teeth in opposing arch, face, head, neck). • Does not cross the midline. • Convergence of afferent neurons. www.indiandentalacademy.com
- 45. Toothache of Maxillary Sinus/Nasal Mucosa Origin Origin Infection of the maxillary sinus or inflammation of nasal mucosa. Clinical Characteristic s Constant dull ache or pressure; sensitivity to cold, percussion, chewing; pain in multiple teeth; pain increased by bending body forward; sinus tender to palpation; Water’s may show air-fluid level. Local Anesthesia Topical anesthesia of nasal mucosa relieves pain in anterior teeth; infiltration anesthesia of posterior teeth relieves pain. Treatment Antibiotics, antihistamine with a decongestant, analgesic. www.indiandentalacademy.com
- 46. Toothache of Myofascial Origin Origin Referral of pain from myofascial trigger points in muscles of mastication – primarily masseter, temporalis, anterior digastric. Clinical Characteristic s Nonpulsatile; constant, aching; variable and cyclic; pain increases with stress and use of offending muscles. Local Anesthetics Anesthetic block of tooth does not alter pain; anesthetic injection of trigger point relieves pain. Treatment Treatment and elimination of trigger points by spray and stretch, injection, or physical therapy. www.indiandentalacademy.com
- 48. Toothache of Neuropathic Origin (Trigeminal Neuralgia) Origin Abnormal function of nerves that innervate teeth (mandibular and maxillary branch of the trigeminal nerves). Clinical Characteristic s Unilateral, severe, paroxysmal bursts of electric-like shocks stimulated by minor superficial provocation; may be felt in teeth; asymptomatic between episodes. Local Anesthetics Topical anesthetic of mucosal or skin “trigger” blocks pain; anesthetic block of nerve root blocks pain. Treatment Referral to neurologist or neurosurgeon. www.indiandentalacademy.com
- 49. Toothache of Neuropathic Origin [Atypical Odontalgia (Phantom Pain)] Origin Not definitely known; most probably a deafferentation pain after trauma. Clinical Characteristic s Constant pain with no obvious pathology; burning, aching pain in molar/premolar area longer than 4 months; local provocation not reliably effect pain. Local Anesthetics Equivocal response Treatment Tricyclic antidepressants, gabapentin www.indiandentalacademy.com
- 50. Toothache of Neurovascular Origin (Tooth migraine) Origin Neurogenic inflamation in the trigeminovascular system Clinical Characteristic s Maxillary canines/premolars; no dental cause; throbbing, episodic, persistent, recurrent pain; dental treatment may provide temporary relief; may become widespread. Local Anesthetics Effects are unpredictable. Treatment Same as for migraine headache; NSAIDs, beta blockers, ergotamines. www.indiandentalacademy.com
- 51. Toothache of Cardiac Origin Origin Myocardial ischemia with regional referral of pain. Clinical Characteristic s Periodic dull pressure of aching in the mandible or teeth; may accompany pain in chest or arm; history of angina; pain precipitated by exercise, stress, or physical activity. Local Anesthetics Anesthesia of teeth not effective. Treatment Refer to medical physician www.indiandentalacademy.com
- 52. Toothache of Psychogenic Origin Origin Psychogenic origin. Clinical Characteristic s Bizarre behavior; history of psychiatric treatment; migratory pain in multiple teeth, frequently bilateral; unexpected or inappropriate response to treatment. Local Anesthetics Equivocal effects. Treatment Refer to psychiatrist. www.indiandentalacademy.com
- 53. Non-Odontogenic Toothaches Warning Symptoms- Summary 1. Spontaneous multiple toothaches 2. Inadequate local dental cause for the pain 3. Stimulating, burning, non-pulsatile toothaches 4. Constant, unremitting, non-variable toothaches 5. Persistent, recurrent toothaches 6. Local anesthetic blocking of the offending tooth does not eliminate the pain 7. Failure of the toothache to respond to reasonable dental therapy www.indiandentalacademy.com
- 54. Differential diagnosis of Primary deep somatic pain of dental origin • Heterotopic referred pains and secondary hyperalgesias as secondary effects of deep pain originating in the following somatic structures: musculoskeletal, vascular, cardiac , or sinus mucosa • Neuropathic pains • Somatoform pain disorders • Heterotopic pains of central origin www.indiandentalacademy.com
- 55. SOMATIC PAIN DEEP PAIN Visceral pain • Pulpal pain • Glandular,Occular and Auricular pain • Neurovascular pain • Vascular pain • Visceral mucosal pain www.indiandentalacademy.com
- 56. GLANDULAR , OCCULAR AND AURICULAR PAIN www.indiandentalacademy.com
- 57. Ocular pain Ophthalmic pain results from stimulation of pain fibers relating either directly or indirectly to the orbit and can be classified as ocular, orbital, or referred. Ocular pain: • Corneal irritation or damage is associated with local pain, photophobia, and lacrimation. • Anterior scleritis presents with severe ocular pain, while posterior scleritis is characterized by less well-defined orbital pain. • Either may be associated with a systemic collagen vascular disease. • A triad of red eye, increased intra-ocular pressure, and mid-dilated pupil is pathognomonic of acute angle glaucoma. www.indiandentalacademy.com
- 58. Orbital pain: • Orbital cellulitis presents acutely with pain exacerbated by palpation and movement. • Orbital pseudotumor is an inflammatory process of unknown etiology that presents with pain, chemosis, diplopia, and red eye. Referred pain: • Occasionally, pain from the area of the greater occipital nerve may radiate to the eye and face, due to convergence and communication between the cervical nerves, and the trigeminal sensory complex. • Migraine, cluster headache, sinusitis, otitis, mastoiditis, temporal giant cell arteritis, and dental pain can be referred to the eye. www.indiandentalacademy.com
- 59. Auricular • Otitis media presents with dull aching or sudden exquisite pain, with or without aural discharge, inflamed tympanic membrane, and systemic evidence of infection. • Otitis externa can be exquisitely painful and is generally an acute process. • Mastoiditis and otitis pain may be referred to the eye, pharynx, and neck due to involvement of multiple cranial and cervical nerves, and convergence into the trigeminal sensory complex. • A common cause of otalgia that is frequently overlooked is referred myofascial pain from muscles of the neck,pharynx, and face www.indiandentalacademy.com
- 60. Salivary Gland Disorders • The salivary glands can be affected by many diseases, including ductal obstruction,infection, inflammation, cystic degeneration, and tumor growth. • Pain and tenderness are typically found in association with ductal obstruction, inflammation,or infection. • Etiology. The most common causes are mumps and acute parotitis in children and blockage of salivary flow by a mucus plug or a sialolith in adults. www.indiandentalacademy.com
- 61. • Salivary gland pain is typically localized to the gland itself, and the gland is tender to palpation. • Precipitating and aggravating factors to the pain are salivary production prior to meals, eating, and swallowing. • Mouth opening may aggravate the pain because of pressure on the gland from the posterior border of the mandible during this movement. • Associated symptoms include salivary gland swelling and, occasionally, fever and malaise. Salivary flow from the affected gland may be minimal or nonexistent. www.indiandentalacademy.com
- 62. SOMATIC PAIN DEEP PAIN Visceral pain • Pulpal pain • Glandular,Occular and Auricular pain • Visceral mucosal pain • Neurovascular pain • Vascular pain www.indiandentalacademy.com
- 63. PAINS EMANATING FROM VISCERAL MUCOSA www.indiandentalacademy.com
- 64. Sinus and Paranasal Pain The most common extraoral source of dental pain arises from the maxillary sinus and associated pain-sensitive nasal mucosa. Symptoms. • Infection and inflammation of the sinuses rarely cause facial pain or headache. • Chronic sinusitis may cause symptoms of fullness or pressure but rarely pain. • A history of increased pain at altitude • Patients may also complain of a “stuffy nose,” blood- or pus-tinged mucus, postnasal drip, fever, and malaise. www.indiandentalacademy.com
- 65. • Frequently, pain is exacerbated by leaning the head forward. • Medial orbital pain with radiation to the temple is a feature of ethmoid sinusitis. • Frontal sinusitis features forehead pain and headache • Maxillary sinusitis is suggested by pain over the upper teeth or orbit. www.indiandentalacademy.com
- 66. • The teeth feel elongated and tender • The maxillary teeth are hypersensitive to cold fluids. • Occasionally, all of the maxillary teeth on the involved side, to the midline, feel uncomfortable and elongated. • The pain is mild but deep and nonpulsating, radiates out of this area onto the face, upward toward the temple, and forward toward the nose. • Cutaneous hyperalgesia along the side of the face and scalp may also be present. www.indiandentalacademy.com
- 67. • The diagnosis of maxillary sinusitis may be confirmed by spraying 4% lidocaine anesthetic from a spray bottle into the nostril on the affected side. This will anesthetize the sensitive area around the ostium. • The pain from the congested nasal mucosa and accompanying maxillary sinusitis should be substantially reduced within a minute or two. www.indiandentalacademy.com
- 68. Treatment • Complete diagnosis and treatment of maxillary sinusitis are left to the ENT specialist. • Treatment usually consists of the use of decongestants and analgesics. • If there is persistent purulent discharge, cultures should be taken and appropriate antibiotics prescribed. www.indiandentalacademy.com
- 69. SOMATIC PAIN DEEP PAIN Visceral pain • Pulpal pain • Glandular,Occular and Auricular pain • Visceral mucosal pain • Vascular pain • Neurovascular pain www.indiandentalacademy.com
- 70. Vascular Pain Temporal Arteritis • Burning, temporal, throbbing, sharp, intermittent, then continuous. • May be associated with loss of visual acuity. • Polymyalgia Rheumatica. Associated fever, weight loss. • Teatment: Prednisolone 60 mg/day. Reducing doses after 5 days. • Rheumatology referral mandatory. www.indiandentalacademy.com
- 71. Carotidynia • Carotid Artery stimulation of various parts of the carotid artery in the region of the bifurcation has been shown to cause pain in the ipsilateral jaw, maxilla, teeth, gums, scalp, eyes, or nose. • In the absence of other demonstrable pathology, unilateral dull, aching, sometimes throbbing pain in the jaws, temple, and neck may be attributable to a carotid system arteritis, also known as carotidynia (carotid pain). www.indiandentalacademy.com
- 72. • The patient with carotidynia will most likely complain of constant or intermittent dull, aching, rarely pulsing jaw and neck pain, with intermittent sore throat or swollen glands. • The pain may also involve the temple and TMJ region and Radiate forward into the masseter muscle with occasional Concomitant tenderness and fullness. • Aggravating factors may include chewing, swallowing, bending over, or straining. www.indiandentalacademy.com
- 73. Treatment. • Medications used in the treatment and prevention of migraine headaches have been shown to be effective in controlling the symptoms of carotidynia. • Steroids and NSAIDs. • Concomitant treatment of any myofascial TrPs will ameliorate the symptoms to some extent. www.indiandentalacademy.com
- 74. SOMATIC PAIN DEEP PAIN Musculoskeletal pain • Periodontal pain • Muscle Pain • Soft connective tissue pain • Osseous and periosteal pain • Temporomandibular joint pain www.indiandentalacademy.com
- 75. Muscle Pain Types of masticatory muscle pain- • Co-contraction • Delayed onset muscle soreness • Myofascial pain • Muscle spasm pain • Muscle inflammation pain www.indiandentalacademy.com
- 76. Muscle co-contraction • Protective co-contraction is a CNS response to injury or threat of injury • In the presence of an injury or threat of injury, normal sequencing of muscle activity seems to be altered to protect the threatened part from further injury. www.indiandentalacademy.com
- 77. • The etiology of protective co-contraction can be any change in sensory or proprioceptive input from associated structures. • Protective co-contraction can also be caused by any source of deep pain input or an increase in emotional stress • The key to identifying co-contraction is that it immediately follows an event and therefore the history is very important. Protective co-contraction only lasts a few days. If it is not resolved, an acute myalgic disorder is likely to follow. www.indiandentalacademy.com
- 78. Myositis • Myositis is an inflammation of the muscle due to a local cause such as trauma, strain, or infection. Symptoms include swelling, tenderness to palpation, and pain with function . Muscle spasm • Muscle spasm is a sudden, involuntary contraction of a muscle or group of muscles, accompanied by pain, limited vertical opening of the mandible, and tenderness to palpation. www.indiandentalacademy.com
- 79. Myofascial pain • Myofascial pain, a common chronic muscular pain disorder is a regional aching pain associated with localized tenderness in firm bands of muscle and tendons called trigger points (TrPs). • Myofascial TrPs can develop in masticatory and associated head and neck muscles secondary to prolonged muscle tension, protracted muscle spasm, forward head posture, parafunctional activity,and trauma. • Factors such as sleep disturbances, joint problems, viral diseases, and metabolic disturbances that weaken a muscle often predispose a weakened muscle to the development of TrPs. www.indiandentalacademy.com
- 80. • The key to diagnosing myofascial pain is to identify a TrP. When palpated, active TrPs cause referred pain in predictable patterns to a known reference zone and are often associated with secondary excitatory effects. • Continuous, dull pain and localized tenderness in one or more muscles are characteristics of myofascial pain, but the severity of pain may range from mild to agonizing, excruciating, or incapacitating. • In early stages, the pain may be more localized, but with chronicity, the TrP can refer pain to more distant sites . www.indiandentalacademy.com
- 81. PSYCHOPHYSIOLOGIC THEORY OF MPD PSYCHOLOGICAL STRESS ↓ MUSCLE HYPERACTIVITY ↓ MUSCLE FATIGUE ↓ MYOSPASM ↓ MPD www.indiandentalacademy.com
- 82. DIAGNOSTIC FEATURES OF THE MPD PATIENT Unilateral, dull, aching facial pain that is poorly localized Moderate to severe limitation of mouth opening No TMJ tenderness Muscle tenderness (masticatory and cervical) No radiographic TMJ changes www.indiandentalacademy.com
- 83. GENERAL CHARACTERISTICS OF MPD PATIENTS Predominately females 20–40 year age group Frequent history of other psychophysiologic diseases Often suffer from chronic depression Seek multiple care providers Have difficulty accepting a psychophysiologic etiology for their problem www.indiandentalacademy.com
- 84. HOME THERAPY Check for clenching habits Limitation of jaw movement Soft non-chewy diet Moist heat and massage of the jaw muscles www.indiandentalacademy.com
- 85. Physical therapy • Massage/myofascial release/muscle energy • Manipulation techniques • Spray and stretch • Heat/cold treatments • Surface stimulation techniques: TENS etc. • Relaxation/biofeedback techniques www.indiandentalacademy.com
- 86. MPS: Pharmacological Approaches • Antidepressants • Traditional muscle relaxants • GABA agents (baclofen) • Non opioid analgesics • Opioid analgesics www.indiandentalacademy.com
- 87. • Acupressure • Acupuncture • Trigger point injections • Botulinum Neurotoxin injections www.indiandentalacademy.com
- 88. SOMATIC PAIN DEEP PAIN Musculoskeletal pain • Periodontal pain • Muscle Pain • Temporomandibular joint pain • Soft connective tissue pain • Osseous and periosteal pain www.indiandentalacademy.com
- 89. TMJ 1. Ligamentous pain 2. Retrodiscal pain 3. Capsular pain 4. Artritic pain www.indiandentalacademy.com
- 90. 1.Ligamentous pain CLASSIFICATION OF INTERNAL DERANGEMENTS Anteriorly displaced disc that returns to normal position during mouth opening (clicking) Anteriorly displaced disc that does not return to normal position during mouth opening (locking) Adhesion of the disc to the joint socket (locking) www.indiandentalacademy.com
- 94. MEDICAL MANAGEMENT OF PAINFUL TMJ CLICKING Medications for relief of pain Soft, nonchewy diet Use of a bite appliance to prevent chronic tooth clenching and grinding www.indiandentalacademy.com
- 95. SURGICAL TREATMENT OF PAINFUL TMJ CLICKING Arthroscopic surgery Discoplasty (surgical repositioning of the disc) www.indiandentalacademy.com
- 96. TREATMENT OF TMJ LOCKING Arthrocentesis Surgical treatment of TMJ locking Arthroscopic surgery Discoplasty (surgical repositioning of the disc) Discotomy (surgical removal of the disc) www.indiandentalacademy.com
- 97. 2.Retrodiscal Pain • If condylar encroachment occurs on the retrodiscal tissues then inflammation may occur • Acute retrodiscitis- may occur due to trauma to mandible • An insidious chronic form of retrodiscitis may occur as a result of functional encroachment of the condyle on the retrodiscal tissues due orthopedic instability that displaces the condyle posteriorly when the teeth are clenched firmly in maximum intercuspation. www.indiandentalacademy.com
- 98. Clinical symptoms of retrodiscal pain • The pain is accentuated by clenching the teeth in maximum intercuspation. • Such pain is decreased by biting against a separator that prevents intercuspation of the teeth. • The pain is accentuated by forced ipsilateral excursive movement of the mandible. • Pain is not induced by resisted protrusion of the mandible. • Dysfunction may be displayed as acute malocclusion in the resting occluded position. • Secondary central excitatory effects may be displayed. www.indiandentalacademy.com
- 99. 3.Capsular pain • Capsular pain results from inflammation of the synovial and fibrous capsules, which is referred to as synovitis and capsulitis, respectively. • Synovitis may result from localized trauma, abusive use, toxemias, specific infection, or as an allergic response. It frequently occurs as a manifestation of arthritis. • Capsulitis may result from acute trauma or from intrinsic strains that injure the capsular ligament www.indiandentalacademy.com
- 100. Capsular pain - Clinical Features • Palpable tenderness directly over the condyle. • Occasional palpable fluctuant swelling over the joint proper. • The pain is accentuated by translatory movements that stretch the capsule. • There is no increase in pain by clenching the teeth, nor is there any alteration in pain by biting against a separator. • Dysfunction occurs in the form of restricted mandibular movement, especially in extended ranges. Most restriction is due to the inhibitory influence of pain. Joint stiffness and strange joint sounds may occur during the first few movements following periods of inactivity. Acute malocclusion may occur as the result of increased intracapsular fluid. • Secondary central excitatory effects may be displayed. www.indiandentalacademy.com
- 101. 4.Arthritic Pain • Osteoarthritis • Osteoarthrosis • Rheumatoid arthritis • Uraemic arthritis • Traumatic arthritis www.indiandentalacademy.com
- 102. Arthritic Pain The following are clinical symptoms by which arthritic pain can be recognized: • There is usually some degree of capsular pain as well as other symptoms of synovitis/capsulitis. • The pain is accentuated by biting pressure, fast movements, and forced movements. • The pain is decreased by biting against a separator on the ipsilateral side • The pain is increased by biting against a separator on the contralateral side.www.indiandentalacademy.com
- 103. • Dysfunction is expressed as restricted movement, interference during movements, and acute malocclusion. Restricted movement may be due to inflammatory swelling, capsular inflammation, altered synovial fluid function,and the inhibitory influence of pain(muscle co- contraction). Interference during movement results from damaged articular surfaces or condyle-disc complex impairment. Acute malocclusion may be due to increased intracapsular fluid or osseous change. www.indiandentalacademy.com
- 104. SOMATIC PAIN DEEP PAIN Musculoskeletal pain • Periodontal pain • Muscle Pain • Temporomandibular joint pain • Osseous and periosteal pain • Soft connective tissue pain www.indiandentalacademy.com
- 105. OTHER MUSCULOSKELETAL PAINS Osseous and periosteal pain • The other musculoskeletal pains of the face and mouth include osseous pains, periosteal pains, and soft connective tissue pains . • Since osseous structures and soft connective tissue are less intimately related to biomechanical function, they are less well-innervated proprioceptively and therefore are less localizable subjectively. • Also, pains emanating from such structures are less likely to induce muscle effects. www.indiandentalacademy.com
- 106. Osseous Pains • Pains that emanate from the bony structures of the mouth and face exclusive of the periodontal structures and the temporomandibular joints constitute another subdivision of musculoskeletal pain. • Pains from this source are predominantly inflammatory as a result of injury, infection, or surgical intervention. www.indiandentalacademy.com
- 107. • There is minimal dysfunction other than that due to the inhibitory influence of pain. Secondary factors, however, such as muscle co-contraction, local muscle soreness, myospasm, or cellulitis may contribute to some dysfunction. www.indiandentalacademy.com
- 108. Dry-Socket Pain • A frequent osteitic involvement of the mouth is dry-socket that follows tooth extraction. • This condition is the result of inflammation of remnants of the periodontal ligament and cortical bone of the alveolus. • Being components of a fibrous joint, these structures are richly innervated with both mechanoreceptors and nociceptors. www.indiandentalacademy.com
- 109. • They therefore have the propensity to initiate reactive muscle effects and considerably more nociceptive response than do other osseous structures. • Protective muscle co-contraction as well as secondary central excitatory effects are frequent complications. • Referred pain involving many teeth, spots of touchy gingiva or skin, areas of deep palpable tenderness, and secondary masticatory muscle soreness may be displayed. • Dry-socket pain may also initiate a myofascial trigger point pain mechanism especially affecting the masseter and temporalis muscles. www.indiandentalacademy.com
- 110. Periosteal Pains • The periosteum, in contrast to bone, is richly innervated with sensory receptors. • It is particularly sensitive to pressure and impact stress. • The mechanoreceptors in periosteal tissue supply proprioceptive input for underlying bony structures. • Noxious stimulation of the periosteum therefore has a high potential for reactive muscle effects and nociception. • The pain that emanates from the periosteum is disproportionately greater than the initiating noxious stimulus. www.indiandentalacademy.com
- 111. SOMATIC PAIN DEEP PAIN Musculoskeletal pain • Periodontal pain • Muscle Pain • Temporomandibular joint pain • Osseous and periosteal pain • Soft connective tissue pain www.indiandentalacademy.com
- 112. Soft Connective Tissue Pains • Pain that emanates from the soft connective tissue structures of the mouth and face constitutes a major subdivision of musculoskeletal pain. • Pains from these structures are predominantly inflammatory and relate to other signs of inflammation by which the source of pain may be identified. • The pain is considerably more constant than muscle pain and it usually follows an inflammatory time frame. www.indiandentalacademy.com
- 113. • Acute cellulitis is usually evident from the swelling and pain, and no diagnostic problem occurs as long as the inflammation is located in accessible regions • Subacute and chronic cellulitis is less dramatic and may present diagnostic problems of differentiation from cysts and tumors. • The history and clinical course plus manual palpation and surgical aspiration are the usual means of establishing the diagnosis. • Pain of cellulitic origin should be differentiated from muscle pain, vascular pain, and glandular pain. Other conditions that may initiate soft connective tissue pain are cysts and tumors, both benign and malignant. www.indiandentalacademy.com
- 114. Therapeutic Options For the management of primary deep somatic musculoskeletal pains that emanate from osseous,periosteal, and soft connective tissue structures, the following therapeutic options are available • Analgesics for palliative relief • Reduction of functional demands • counseling • Cause-related therapy consisting of the identification and treatment of causative factors and contributing conditions, and general medical and surgical supportive care including antibiotics, antiinflammatory agents, and deep heat therapy www.indiandentalacademy.com
- 116. Neuropathic Pain 1.Burning-type pains that are spontaneous, triggered, or ongoing and unremitting. 2. The pain occurs disproportionate to the stimulus. 3. The pain is accompanied by other neurologic signs. 4. The pain may be initiated, accentuated, or maintained by sympathetic activity. www.indiandentalacademy.com
- 117. Neuropathic Pain 1)Episodic pain -Paroxysmal Neuralgia pain -Neurovascular pain 2)Continuous pain www.indiandentalacademy.com
- 118. Episodic Neuropathic Pain 1.Quick, sharp, electrical-like pain (paroxysmal). 2. Very intense debilitating pain. 3. Duration is momentary (seconds). 4. Very little to no pain between episodes. 5. The pain follows the distribution of the affected nerve. www.indiandentalacademy.com
- 119. Neuralgias • Trigeminal – Primary (idiopathic) – Secondary (symptomatic) • Acute herpetic and Post herpetic • Geniculate (Ramsay Hunt) • Glossopharyngeal • Superior laryngeal • Occipital www.indiandentalacademy.com
- 120. Trigeminal neuralgia • Trigeminal neuralgia is characterized by sudden, stabbing, and severe unilateral facial pain in ≥1 of the 3 divisions of the trigeminal nerve, most frequently the second. • Onset is frequently triggered by mechanical stimulation such as talking, chewing, or touch. • Attacks can last from seconds to a few minutes. Periods of attacks can last weeks or months, followed by periods of remission for months or years. • Incidence increases with age, with the average onset at age 50 years; it more commonly presents in women. • Limited information is available about the etiology of trigeminal neuralgia other than the possible compression of the trigeminal root by a vessel or tumor. www.indiandentalacademy.com
- 121. Treatment • Carbamazepine is the drug of first choice for treatment, with an initial beneficial response in >75% of patients. • Baclofen potentiates the action of carbamazepine and can be a useful adjunct. • Gabapentin is a safe and well-tolerated adjunct to • Carbamazepine or may be used as sole treatment. Other less frequently used agents include oxcarbazepine, lamotrigine, clonazepam, and sodium valproate. www.indiandentalacademy.com
- 122. • Some of the surgical approaches to the treatment of trigeminal neuralgia include • microvascular decompression • radiofrequency rhizothomy • gamma knife surgery. Microvascular decompression of the trigeminal nerve provides immediate and long-term pain relief in >70% of patients. www.indiandentalacademy.com
- 123. GLOSSOPHARYNGEAL NEURALGIA • Paroxysmal pain that is similar to, though less intense than, the pain of TN. • The location of the trigger zone and pain sensation follows the distribution of the glossopharyngeal nerve, namely, the pharynx, posterior tongue, ear, and infraauricular retromandibular area. • Pain is triggered by stimulating the pharyngeal mucosa during chewing, talking, and swallowing. www.indiandentalacademy.com
- 124. • May be associated with vagal symptoms, such as syncope and arrhythmia, owing to the close anatomic proximity of the two nerves. • The application of a topical anesthetic to the pharyngeal mucosa eliminates glossopharyngeal nerve pain and can aid in distinguishing it from the pain of other neuralgias. • The most common causes of glossopharyngeal neuralgia are intracranial or extracranial tumors and vascular abnormalities that compress CN IX. www.indiandentalacademy.com
- 125. • Treatment is similar to that for TN,with a good response to carbamazepine and baclofen. • Refractory cases are treated surgically by intracranial or extracranial section of CN IX, microvascular decompression in the posterior cranial fossa, or (more recently) by percutaneous radiofrequency thermocoagulation of the nerve at the jugular foramen. www.indiandentalacademy.com
- 126. NERVOUS INTERMEDIUS (GENICULATE) NEURALGIA • Nervous intermedius (geniculate) neuralgia is an uncommon paroxysmal neuralgia of CN VII, characterized by pain in the ear and (less frequently) the anterior tongue or soft palate. • Pain is not as sharp or intense as in TN, and there is often some degree of facial paralysis,indicating the simultaneous involvement of the motor root. www.indiandentalacademy.com
- 127. • Geniculate neuralgia commonly results from herpes zoster of the geniculate ganglion and nervus intermedius of CN VII, a condition referred to as Ramsay Hunt syndrome. • Viral vesicles may be observed in the ear canal or on the tympanic membrane. www.indiandentalacademy.com
- 128. Treatment • A short course (2 to 3 weeks) of high-dose steroid therapy • Acyclovir • Carbamazepine and antidepressants. • Patients who do not respond to these medications may undergo surgery to section the nervus intermedius www.indiandentalacademy.com
- 129. OCCIPITAL NEURALGIA • Occipital neuralgia is a rare neuralgia in the distribution of the sensory branches of the cervical plexus (most Commonly unilateral in the neck and occipital region). • The most common causes (in descending order of frequency) are trauma, neoplasms, infections, and aneurysms involving the affected nerve(s). • Palpation below the superior nuchal line may reveal an exquisitely tender spot. • Treatment has included corticosteroids, neurolysis, avulsion, and blocking the nerve with a local anesthetic www.indiandentalacademy.com
- 130. Superior Laryngeal neuralgia • Superior Laryngeal nerve is a branch of vagus and innervates the cricothyroid muscle of the larynx. • Periodic ,unilateral submandibular pain radiating through the ear, eye or shoulder. • Pain is paroxysmal, lasting momenterily and may be provoked by swallowing,straining the voice,turning the head,coughing,sneezing or blowing the nose. www.indiandentalacademy.com
- 131. Neuropathic Pain 1)Episodic pain -Paroxysmal Neuralgia pain -Neurovascular pain 2)Continuous pain www.indiandentalacademy.com
- 133. Migraine headaches The pathogenesis of migraine headaches is controversial, but current research has implicated a neurogenic etiology (neurogenic inflammation) possibly causing secondary cerebrovascular changes. • Triggering factors Diet, stress, sleep disturbances, and menstruation. • The forms of migraine Migraine with aura Migraine without aura www.indiandentalacademy.com
- 134. • No laboratory or radiological tests exists for migraine and diagnosis is made on the basis of clinical features. • Both forms of migraine have a hereditary predisposition, • Begins at a young age • Primarily affect women • Typical attacks may last from 4–72 hours • Usually unilateral • Pulsating pain with moderate to severe intensity. • Sometimes the pain may be bilateral, especially in children, and non-pulsatile. www.indiandentalacademy.com
- 135. • Associated with symptoms of nausea and/or vomiting, photophobia, and phonophobia. • Often begin immediately after awakening or soon thereafter. • Patients typically are unable to function and just wish to lie down in a dark room. • Migraine with aura is characterized by visual disturbances, such as flashing lights and colors, zigzag patterns, or blind spots and, on occasion, numbness and tingling more on one side of the face and arm . www.indiandentalacademy.com
- 136. Cluster headaches • Although cluster headaches are relatively uncommon, it is one of the most severe forms of headache and facial pain, and has been referred to as a "suicide headache" • Male-to-female ratio of 5:1. • It is of two types: -An episodic type, where the attacks of pain occur during a time of susceptibility, known as the cluster period, which may last for weeks or months -Chronic form, where there is an absence of pain-free remission periods . www.indiandentalacademy.com
- 137. • A cluster attack may last from 15 minutes to 3 hours, and can occur from once every other day to as often as 8 times per day. • Frequently, the patient is awakened from sleep by the attack. • Cluster pain is excruciating and has a boring, sharp, or Burning quality. unilateral in location, involving the periorbital area, often with radiation to the ipsilateral temple and maxilla, including the teeth. • And is associated with autonomic symptoms such as lacrimation from the eye on the affected side, nasal congestion, rhinorrhea, forehead and facial sweating, ptosis, and eyelid edema. www.indiandentalacademy.com
- 138. Tension-type headache Tension-type headache is divided into two major categories: • Episodic-The episodic tension-type headache lasts for 30 minutes to one week • Chronic- form occurs with a frequency of at least 15 days a month for at least 6 months. • Pain is usually described as a steady, dull, aching sensation of mild to moderate intensity, but throbbing pain may occasionally be present. • The headaches occur primarily in the bifrontal occipito- nuchal and bitemporal areas, and are often associated with stiffness and tenderness of the neck. www.indiandentalacademy.com
- 139. • Photophobia or phonophobia may also be part of the headache complaint in some patients. • Unlike migraine, physical activity does not worsen the pain, and nausea is usually absent. • The chronic type may evolve from the episodic type and shares similar clinical features. • Tension-type headaches must be differentiated from migraine without aura, referred pain from myofascial trigger points, cranial arteritis, and TMD, especially when bitemporal pain is a chief complaint. www.indiandentalacademy.com
- 140. Chronic paroxysmal hemicrania • Is short-lasting (2 to 45 minutes) • Frequently occurring attacks of pain (five per day for more than half of the time). • The quality of pain is throbbing or pounding,with an intensity that parallels that of cluster headaches, the patient often choosing to pace the floor during an attack. • Pain location is predominantly oculotemporal and frontal, always on the same side, and can spread to involve the entire side of the head and the neck, shoulder, and arm. Cases involving CPH presenting as intermittent toothache have been reported. www.indiandentalacademy.com
- 141. • Turning or bending the head forward may precipitate an attack in some cases. • Associated symptoms include unilateral lacrimation, nasal stuffiness, and conjunctival injection. • Nausea and vomiting are usually absent, as are visual or somatosensory auras. • In contrast to cluster headache, CPH is seen predominantly in women. • Age at onset appears to be 20 years, www.indiandentalacademy.com
- 142. Chronic Paroxysmal Hemicrania- Treatment • Indomethacin is the medication of choice for CPH. • If the pain does not resolve with this medication, it is unlikely to be CPH. • Aspirin and naproxen have a partial effect, but the relief is not as dramatic as with indomethacin. www.indiandentalacademy.com
- 143. Continuous Neuropathic Pain 1.Quality is often dull, yet burning-type pain. 2. The pain is ongoing and unremitting, yet the intensity can show patterns of fluctuation. 3. The pain is accompanied by other neurologic signs. (anesthesia, paresthesia, hypoesthesia, hyperesthesia) 4. There is normally no evidence of any tissue (somatic) changes or disease. 5. The pain may be initiated, accentuated, or maintained by sympathetic activity.www.indiandentalacademy.com
- 144. Neuropathic Pain 1)Episodic pain -Paroxysmal Neuralgia pain -Neurovascular pain 2)Continuous pain www.indiandentalacademy.com
- 145. Neuropathic Pain: Continuous • Neuritis • Deafferentation • Sympathetically maintained pains www.indiandentalacademy.com
- 146. Neuropathic Toothache: Continuous 1. Neuritis • Inflammatory condition in the peripheral distribution of the nerve due to trauma, chemical, viral or bacterial causes – Arises in the maxillary or mandibular division of the trigeminal nerve along with other neurological symptoms – Neuritis of the superior dental plexus due to extension from maxillary sinusitis may cause a toothache in and around one or more of the maxillary teeth – Neuritis of the inferior alveolar nerve in the mandibular teeth from direct trauma, dental infection or surgery www.indiandentalacademy.com
- 147. Neuritic Pain • Herpes Zoster • Post-herpetic Neuralgia • Peripheral Neuritiis www.indiandentalacademy.com
- 148. Herpes Zoster • It is an acute neuritis of viral source that presents with severe pain in the exact distribution of the involved nerve. • Tiny vesicles appear usually 4-5 days after the onset of the pain and burst open to produce surface lesions. • Unilateral presentation • Ophthalmic division of trigeminal nerve is most commonly affected. www.indiandentalacademy.com
- 149. Post-Herpetic Neuralgia • Patients with PHN experience persistent pain, paresthesia, hyperesthesia, and allodynia months to years after the zoster lesions have healed. • The pain is often accompanied by a sensory deficit, and there is a correlation between the degree of sensory deficit and the severity of pain. www.indiandentalacademy.com
- 150. • The best therapy for PHN is prevention. The use of antiviral drugs, particularly famciclovir, along with a short course of systemic corticosteroids during the acute phase of the disease may decrease the incidence and severity of PHN. • Topical therapy includes the use of topical anesthetic agents, such as lidocaine, or analgesics, particularly capsaicin. • Tricyclic antidepressants- amitriptyline,nortriptyline, doxepin, and desiprimine • Gabapentin • Anticonvulsant drugs, such as carbamazepine or phenytoin. www.indiandentalacademy.com
- 151. • When medical therapy has been ineffective in managing intractable pain, nerve blocks or surgery at the level of the peripheral nerve or dorsal root have been effective for some patients. www.indiandentalacademy.com
- 152. Peripheral Neuritis • It is a painful condition that relates to the entire peripheral nerve trunk,not just the nerve endings and terminal branches. • Sensory ,motor and autonomic symptoms may be present,depending on the fibre content of the affected nerve. • The pain is described as burning, bright, or stimulating, and is usually accompanied by a feeling of paresthesia or anesthesia in the distribution of the affected nerve. www.indiandentalacademy.com
- 153. • Trigeminal neuritis is due to inflammation of the peripheral branches of a nerve trunk as a result of trauma, bacterial or viral infection, or toxic causes. • An example of neuritis affecting the facial nerve is Bell’s palsy, which usually results from compression of the nerve inside the facial canal or Stylomastoid foramen. • It should be noted that the sympathetic nervous system, specifically sympathetic efferent activity, may be involved in various deafferentation pain disorders as well as other neuropathies related to trauma. www.indiandentalacademy.com
- 154. Neuropathic Pain: Continuous • Neuritis • Deafferentation • Sympathetically maintained pains www.indiandentalacademy.com
- 155. Neuropathic Pain: Continuous 2. Deafferentation • Crushing or cutting of a peripheral nerve (Traumatic Neuralgia) – May follow an injury such as external trauma, pulp extirpation, extraction or major oral surgery – Often mistaken for a post-traumatic or postoperative complication www.indiandentalacademy.com
- 156. • When a peripheral nerve is partially or completely severed as a result of trauma injury, it attempts to repair the damage by regenerating. • When this attempt is unsuccessful, a disorganized, intertwined mass of nervous tissue can result. • Neuromas are characterized by deep, aching, burning pain induced by compression or stretching at the site of injury. www.indiandentalacademy.com
- 157. Neuropathic Pain: Continuous Atypical Odontalgia (Phantom Toothache) • Pain is felt in a tooth or tooth site (maxillary canine and premolar are most common) • Pain is continuous or almost continuous • Pain persists more than four months • No sign of local or referred pain • Local anesthetic of the painful tooth provides equivocal results www.indiandentalacademy.com
- 158. Neuropathic Pain: Continuous • Neuritis • Deafferentation • Sympathetically maintained pains www.indiandentalacademy.com
- 159. Sympathetically Maintained Pains Deafferentation tooth pains may be influenced by the efferent activity of the sympathetic nervous system • Normal sympathetic activity (sympathetic tone) can be responsible for maintaining the pain • An increase in sympathetic activity could increase the pain condition • Increased levels of emotional stress could aggravate this condition www.indiandentalacademy.com
- 160. Atypical Facial Pain • Diagnosis of exclusion • Psychogenic facial pain • Location and description inconsistent • Women, 30 – 50 years old • Usually accompanies psychiatric diagnosis • Treat with antidepressantswww.indiandentalacademy.com
- 161. Axis II Categories (Psychologic Conditions) • Psychologic conditions influence all pains. These conditions have their greatest effects on chronic pains. The longer a patient suffers, the greater the influence of these factors. • Psychological intensification of pain may proceed until the suffering is wholly disproportionate to the peripheral nociceptive input. www.indiandentalacademy.com
- 162. • Although the original pain complaint may have displayed the usual clinical characteristics of somatic or neuropathic pain, as psychological intensification converts it into a chronic pain disorder, the clinical symptoms take on identifying features. • Such pain lacks an adequate source of input that is anatomically related to the site of pain. • It may be felt in multiple and sometimes changeable locations. • Pain bilaterally may become evident in the absence of bilateral sources of noxious input. www.indiandentalacademy.com
- 163. • The complaint may display unusual or unexpected responses to therapy. It may respond too quickly or too slowly. It may respond in an exaggerated way or with unusual side effects or complications. • The response may be followed by a relapse without organic justification, or the condition may remain refractory in spite of otherwise effective therapy. • Pains that are greatly influenced by psychologic factors may display changeableness in location, intensity, or temporal behavior without a reasonable, identifiable organic cause. www.indiandentalacademy.com
- 164. Although there are numerous disorders, the following common mental disorders can greatly influence the individual's pain experience: • 1) Mood Disorders • 2) Anxiety Disorders • 3) Somatoform Disorders • 4) an Other category that includes many other mental conditions or psychologic factors that affect the outcome of a medical condition. www.indiandentalacademy.com
- 165. Mood disorders are subdivided into • Depressive disorders, • Bipolar disorders • Mood disorder is due to a medical condition. Anxiety disorders are subdivided into • Generalized anxiety disorders • Posttraumatic stress disorders, • Anxiety disorders that are due to a medical condition. www.indiandentalacademy.com
- 166. Somatoform Disorders are a group of disorders that are characterized by physical symptoms suggesting a physical disorder for which there are no demonstrable organic findings of known physiologic mechanisms. The somatoform disorders are subdivided into • Undifferentiated somatoform disorders • Conversion disorders • Pain disorders • Hypochondriasis. www.indiandentalacademy.com
- 167. The last category is a broad group of mental disorders that may be related to pain conditions. This category includes – • Malingering • Psychological factors affecting a medical condition -personality traits or coping styles -maladaptive health behavior -stress-related physiological responses. www.indiandentalacademy.com
- 168. CONCLUSION An organized approach is necessary to assess and diagnose orofacial pain, since multiple medical and dental specialties are involved in the management of patients. The clinician must be able to correctly diagnose and treat the patient accordingly, or refer the patient to the appropriate specialist. www.indiandentalacademy.com
- 169. REFERENCES • Jeffrey P Okeson,Bell’s Orofacial Pains,5th edition,Quintessence Publishing Co,1995 • Burket’s,Oral Medicine,11th edition,BC decker Inc 2008 • Burket’s,Oral Medicine-Diagnosis and Treatment,9th edition, Lippencott –Raven Publishers 1997. • O. P. Tandon, V. Malhotra, S. Tandon and I. D’silva,Review Article Neurophysiology of pain : Insight to orofacial pain, Indian J Physiol Pharmacol 2003; 47 (3) : 247–69 www.indiandentalacademy.com
- 170. • Ingle and Bakland, Endodontics,5th edition, Chapter 8, Nonodontogenic toothache and chronic head and neck pains ,page no. 287-356, Published by PMPH-USA, 2002 • David J. Alvarez, Pamela G. Rockwell, Trigger Points: Diagnosis and Management,Am Fam Physician 2002;65:653-60 • Jean Schoenen, Differential diagnosis of facial pain ,Acta neurol. belg., 2001, 101, 6-9 • Richard A. PERTES, Differential diagnosis of orofacial pain,october/november 1998 number 5 & 6 volume 65:348–354 www.indiandentalacademy.com
- 171. • Melis M, Secci S. Diagnosis and Treatment of Atypical Odontalgia: A Review of the Literature and two Case Reports. J Contemp Dent Pract 2007 March;(8)3:081- 089. • Sujay A. Mehta, Joel B. Epstein, Charles Greene, Headache Recognition and Management of Headache,J Can Dent Assoc 2006; 72(9):835–9 www.indiandentalacademy.com
