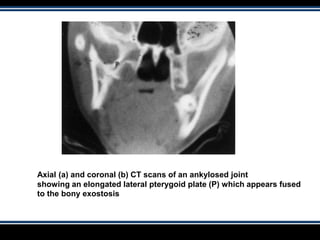
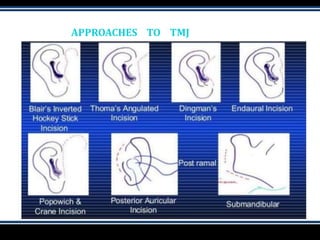
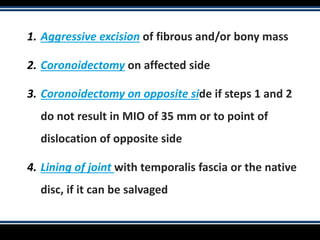
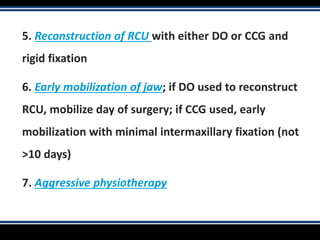
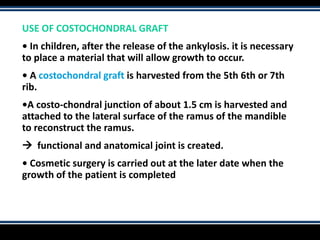
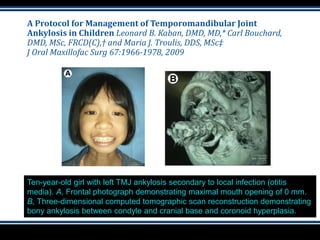
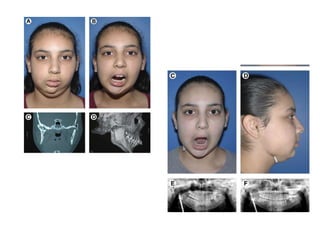
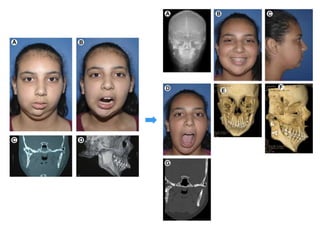
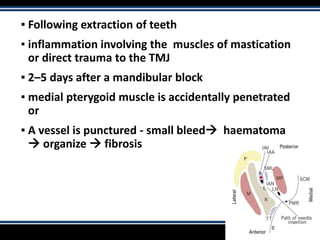
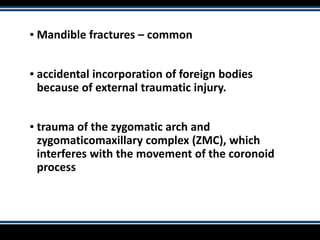
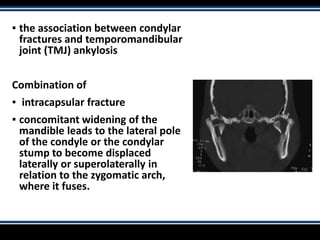
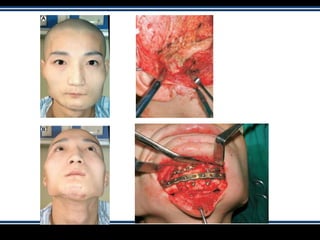
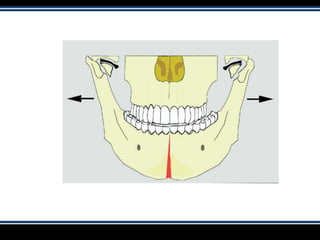
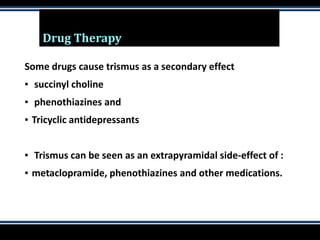
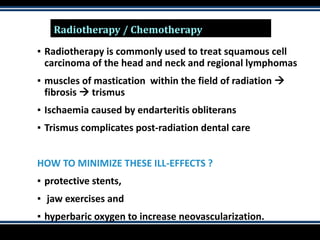
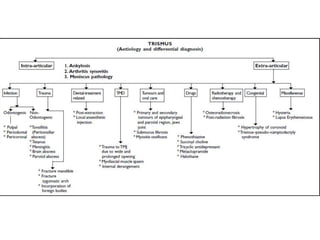
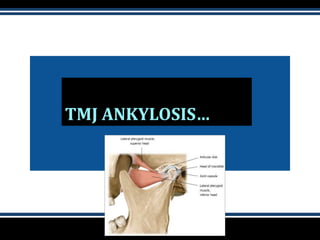
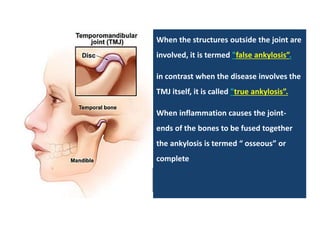
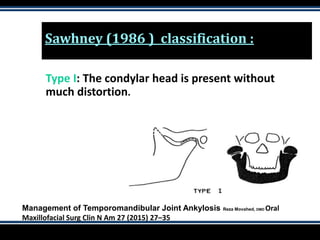
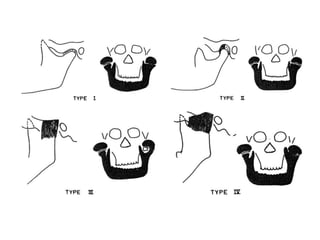
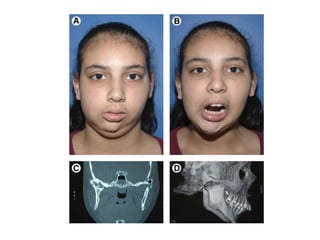
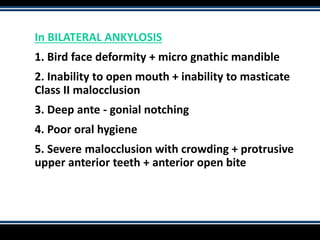
This document provides information on trismus, TMJ ankylosis, their causes and management. It discusses that trismus is the inability to open the mouth, and normal opening is 40-60mm. Trismus can be caused by infections, trauma, dental procedures, tumors, drugs, radiation and congenital issues. TMJ ankylosis is a stiffness of the joint resulting in limited or no mobility. It discusses the classification, clinical manifestations, diagnosis and management of TMJ ankylosis, whether conservative or surgical. The goals of surgical management are to release the ankylosed mass, create a gap for mobility, reconstruct the joint and prevent re-ankylosis.




![1. Interferes with the mastication of food and with
nutrition
2. Prevents oral hygiene and prophylactic care, and
treatment of dental caries
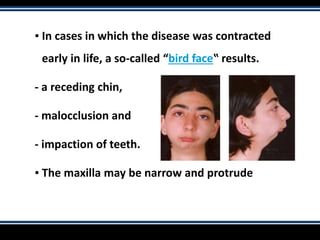
There is destruction of the growth center [situated in the
condyle] and with absence of functional stimulation
prevents normal development of the jaw prevents
normal eruption of the teeth and causes micrognathia](https://image.slidesharecdn.com/trismus-190811164001/85/Trismus-61-320.jpg)