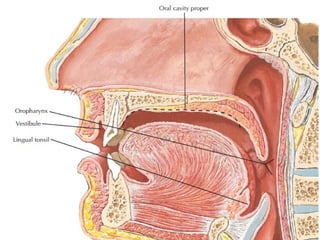
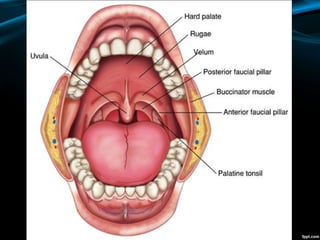
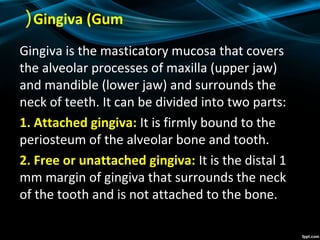
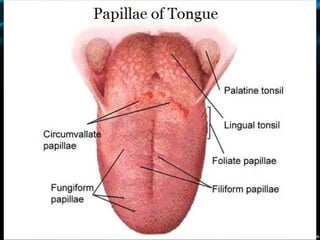
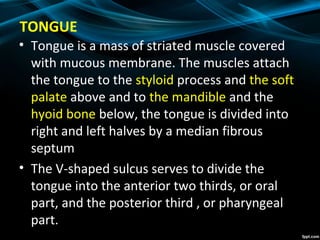
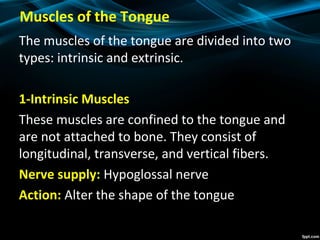
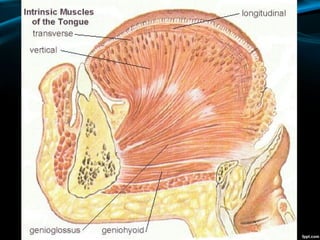
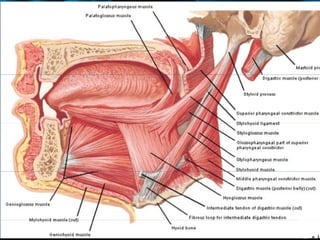
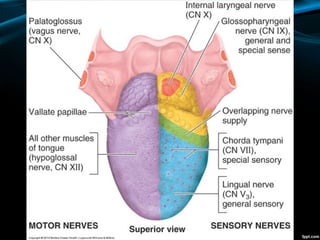
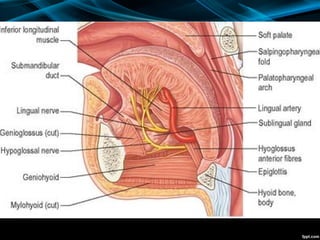
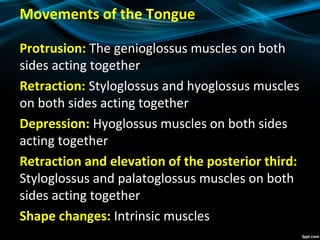
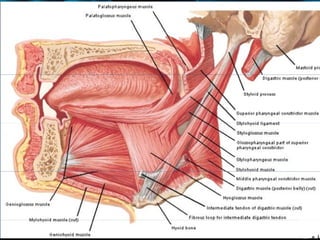
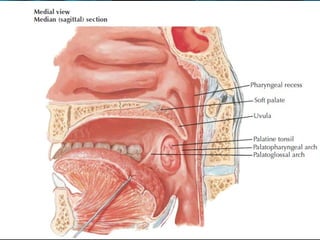
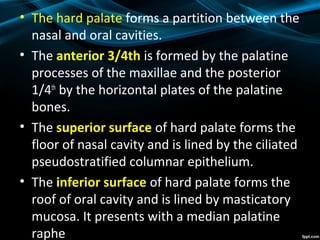
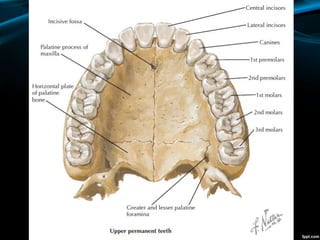
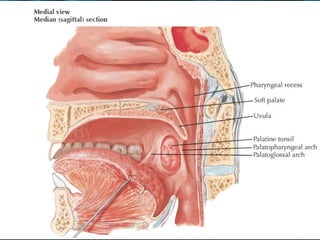
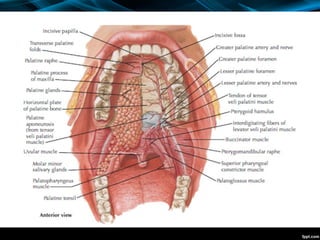
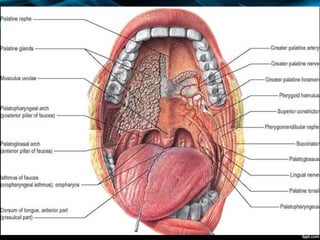
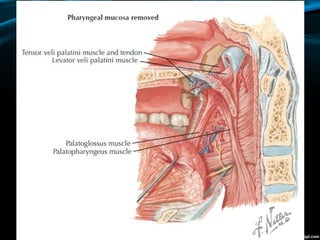
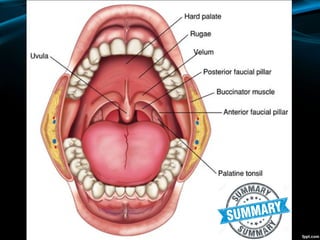
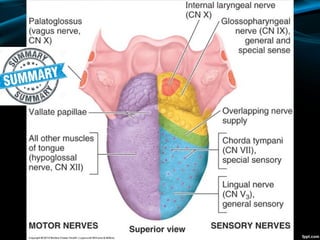
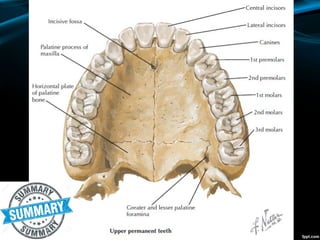
The oral cavity is divided into the oral cavity proper and the vestibule. The oral cavity proper contains the tongue and is bounded by the hard palate and dental arches. The vestibule is the space between the teeth and lips. Other structures include the lips, cheeks, gingiva, palate, and tongue. The tongue contains intrinsic and extrinsic muscles and is innervated by the hypoglossal nerve. The hard palate forms the roof of the mouth while the soft palate hangs from its posterior end and separates the nasal and oral cavities.