The document discusses various topics related to human nutrition:
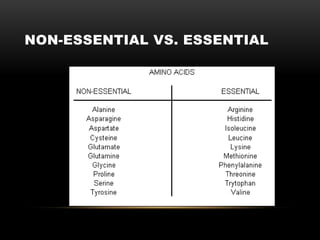
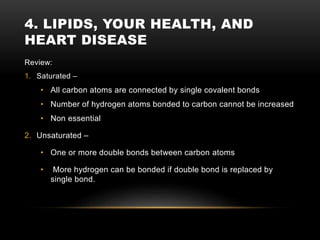
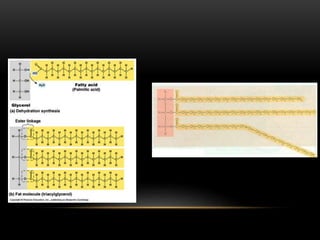
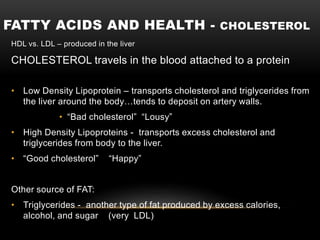
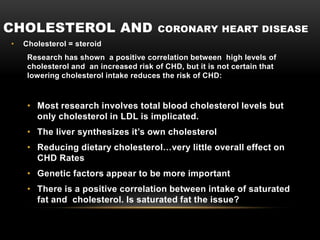
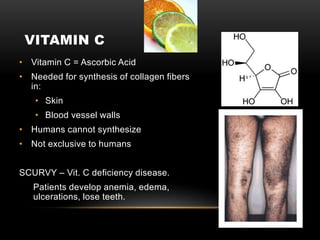
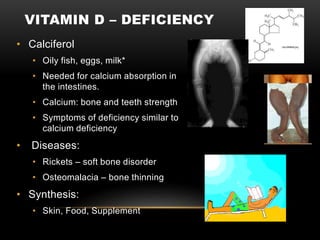
- It describes the essential nutrients that must be consumed as part of our diet, including water, lipids, some amino acids, and vitamins and minerals.
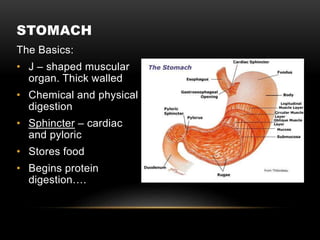
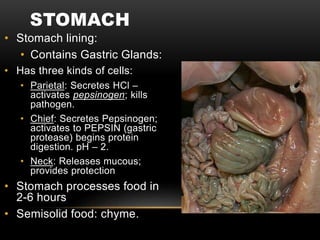
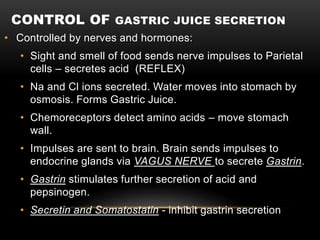
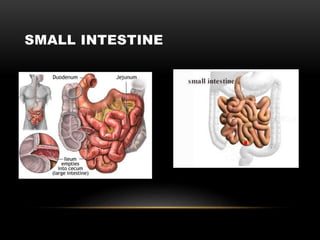
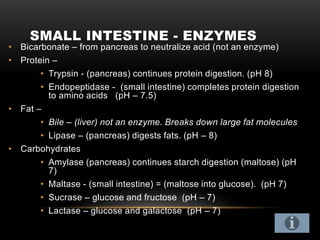
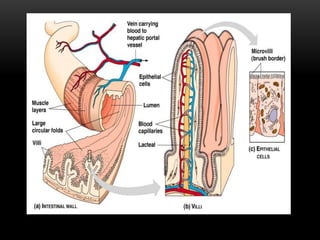
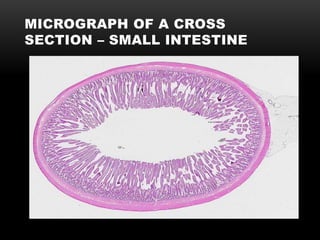
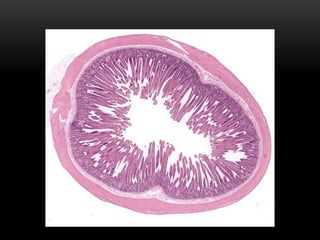
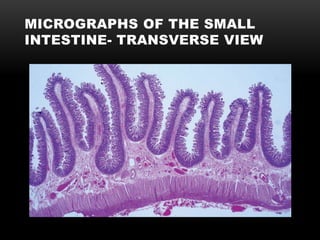
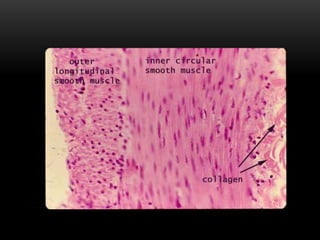
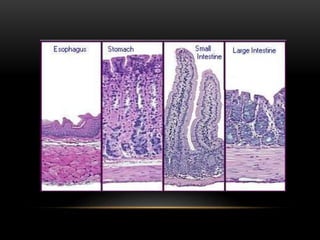
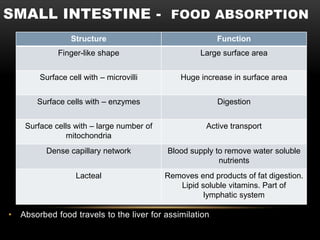
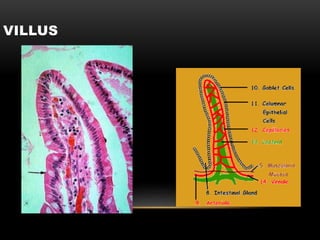
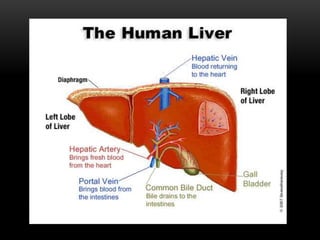
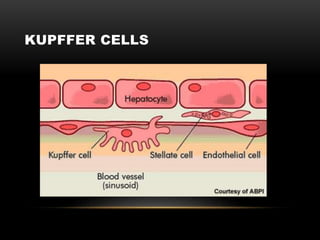
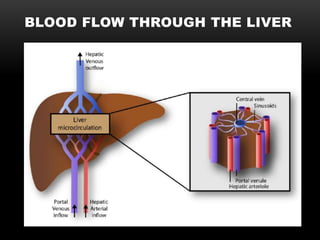
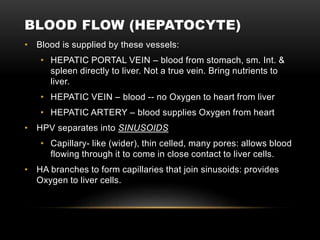
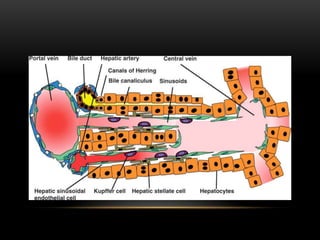
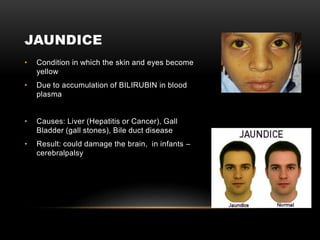
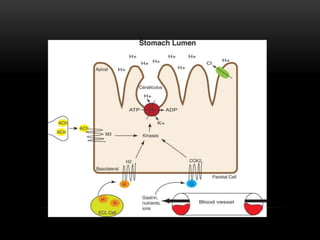
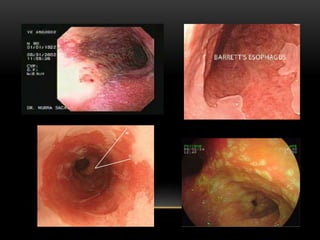
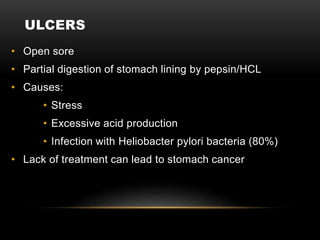
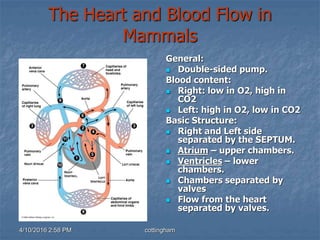
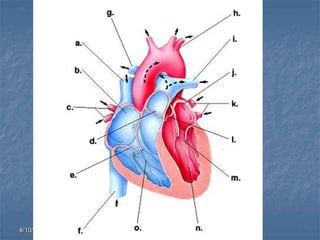
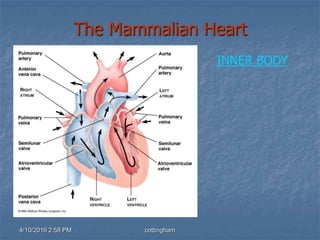
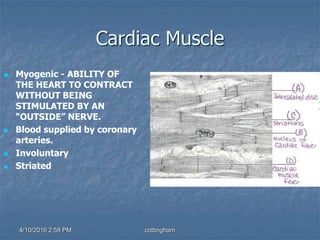
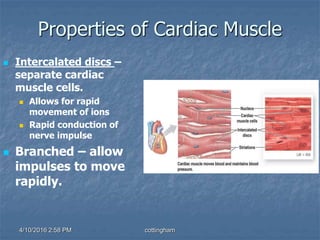
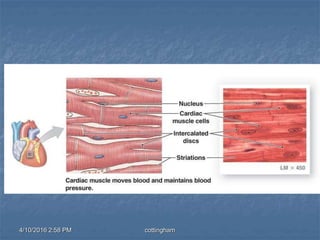
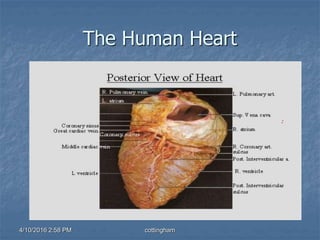
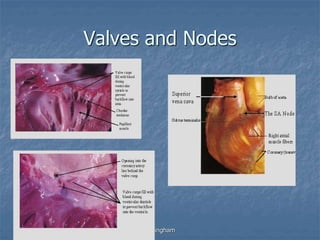
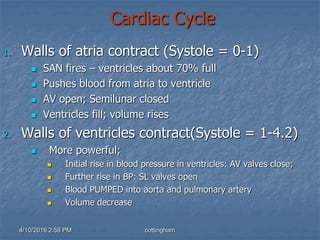
- It then covers digestion, including the roles of the stomach, small intestine, liver, and heart. The stomach aids in protein digestion through gastric juices. The small intestine completes digestion with enzymes from the pancreas and bile from the liver. The liver performs many functions including detoxification and production of proteins and bile. The heart pumps blood throughout the body.