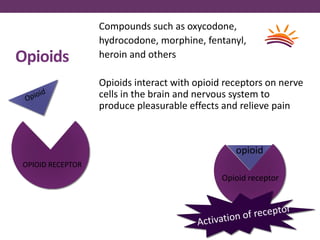
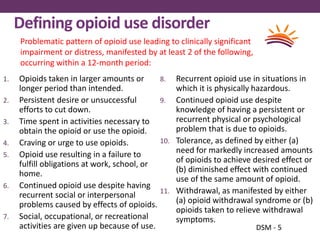
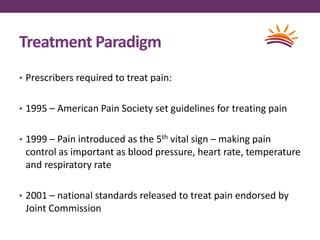
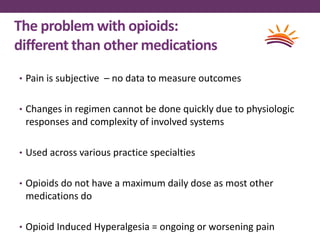
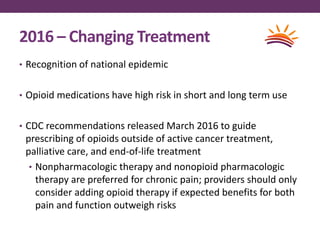
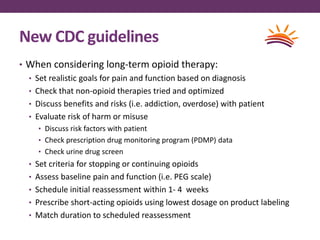
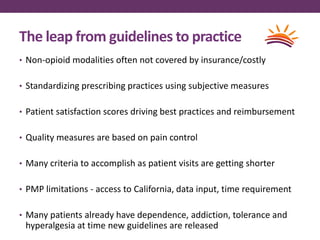
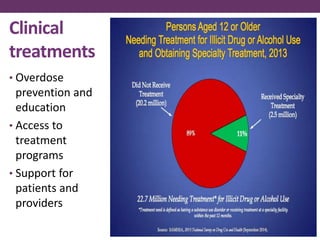
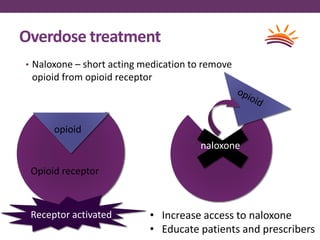
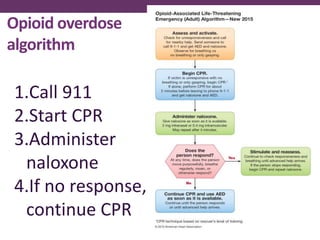
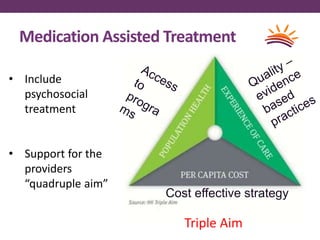
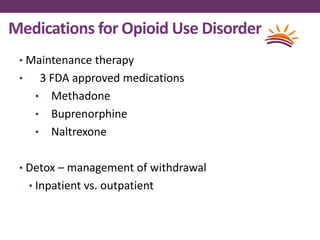
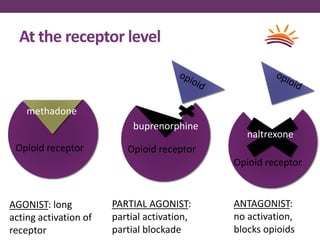
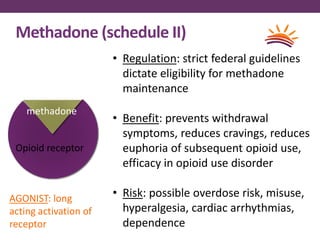
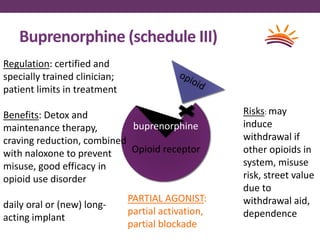
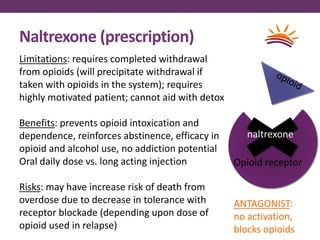
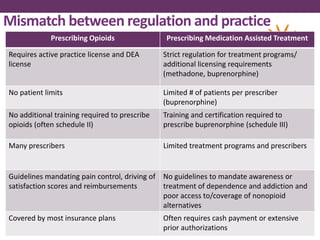
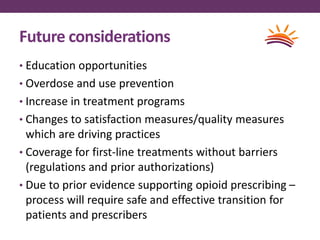
This document outlines options for treating opioid use disorder and dependence. It defines opioid use disorder according to DSM-5 criteria. Treatment options discussed include medication assisted treatment with methadone, buprenorphine, or naltrexone as well as counseling. Regulations around prescribing opioids are more lax than those for treating opioid dependence. The presentation calls for improving access to evidence-based treatments, educating patients and providers, expanding treatment programs, and revising quality measures that may drive over-prescription of opioids.