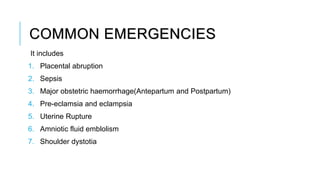
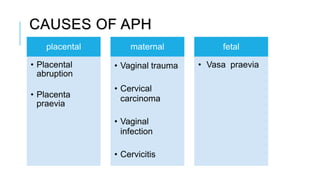
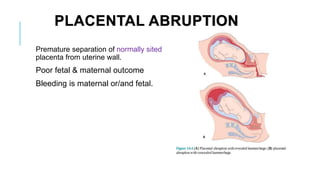
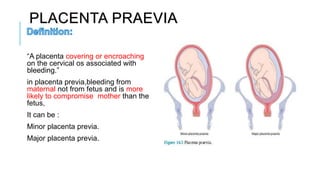
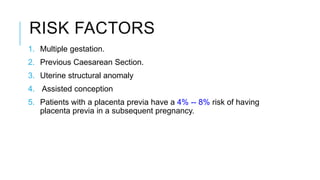
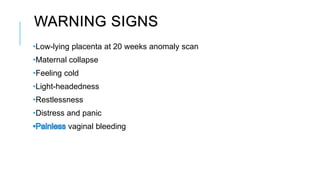
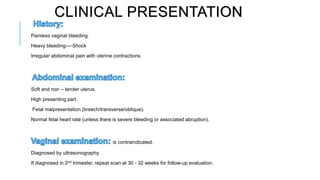
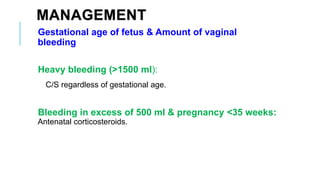
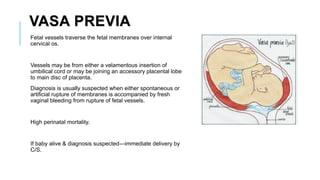
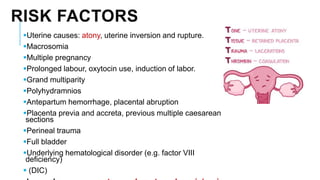
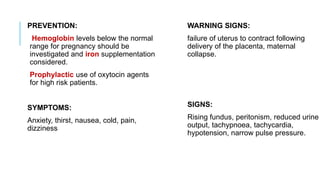
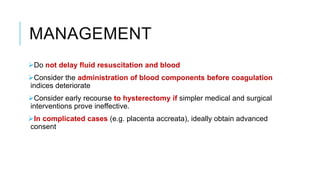
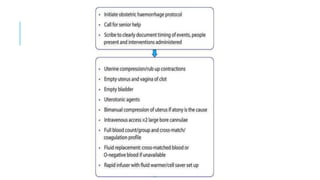
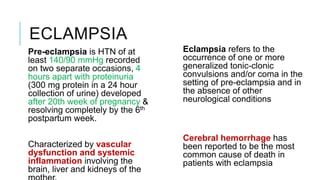
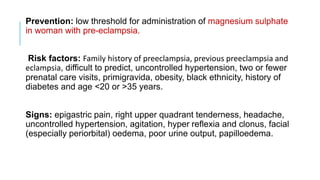
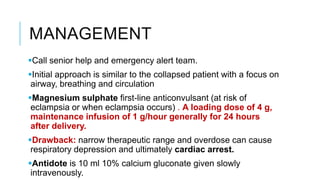
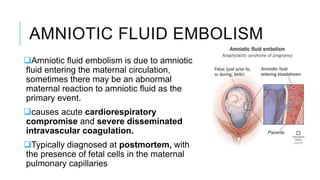
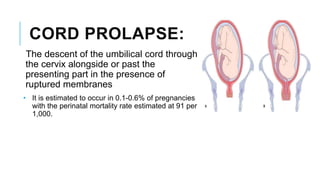
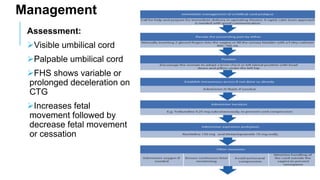
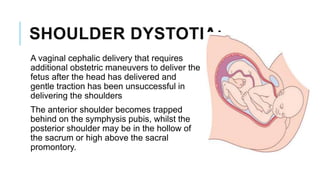
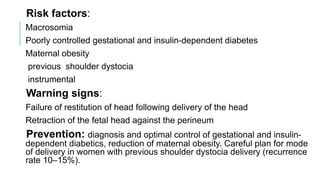
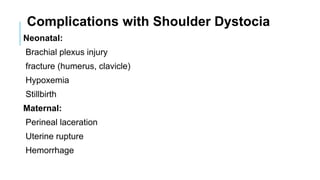
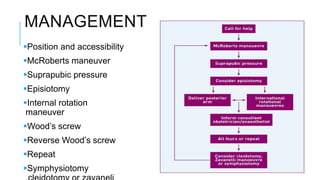
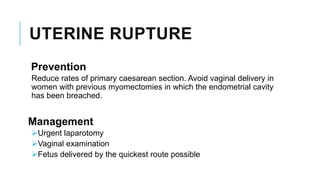
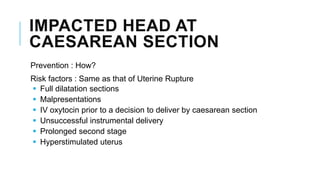
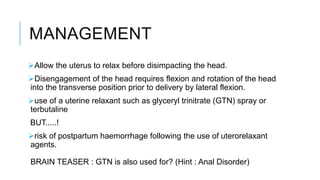
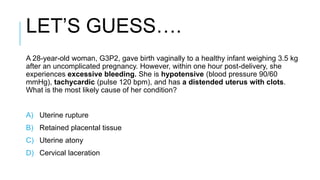
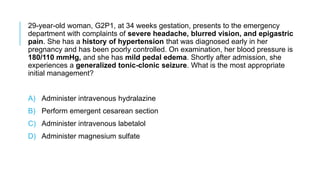
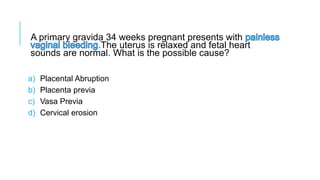
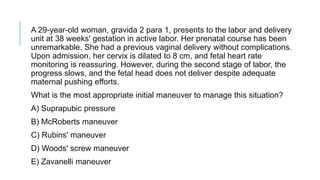
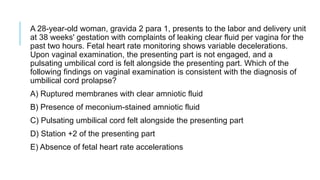
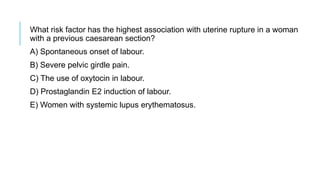
The document outlines common obstetric emergencies, their incidence, risk factors, warning signs, and management strategies, emphasizing conditions such as placental abruption, placenta previa, postpartum hemorrhage, and eclampsia. It also discusses the importance of recognizing early warning signs and provides a stepwise approach for managing emergencies to prevent maternal and fetal morbidity and mortality. Furthermore, it highlights key assessment and management techniques for various obstetric complications.