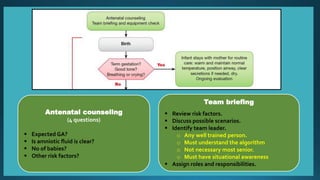
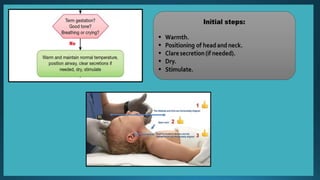
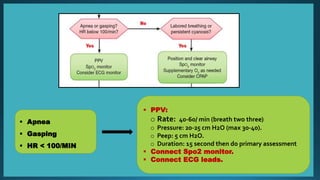
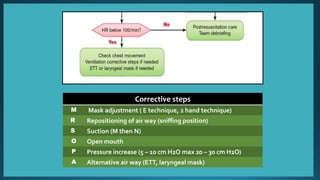
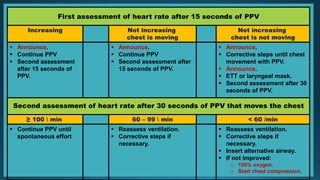
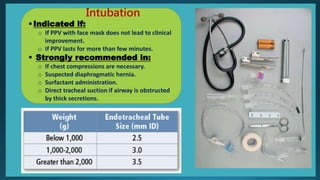
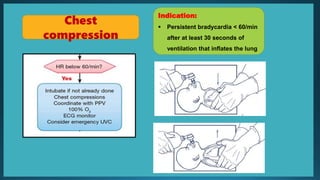
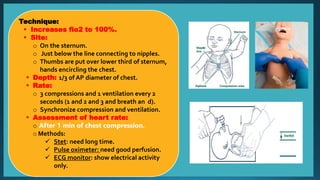
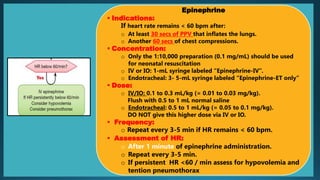
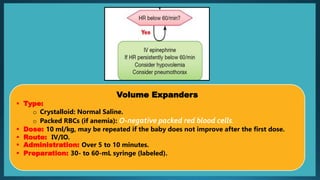
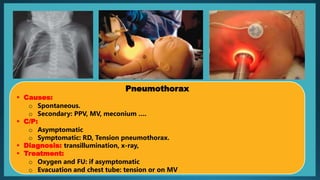
This document outlines a neonatal resuscitation algorithm. It describes assembling a resuscitation team that includes at least one qualified individual for routine births and two for high-risk births. The algorithm then details assessing the newborn at birth and providing positive pressure ventilation if needed. It provides corrective steps if ventilation is inadequate and describes assessing the heart rate after 15-30 seconds. For persistent bradycardia, the steps are chest compressions, epinephrine, and volume expanders. Intubation is indicated if ventilation with a mask is ineffective. The document provides details on techniques and dosages for interventions.