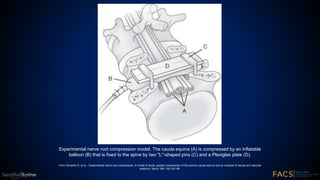
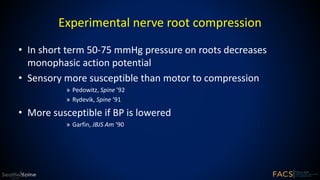
This document summarizes the pathophysiology of nerve root compression. It discusses two main mechanisms: mechanical deformation of nerve roots and the effect of nucleus pulposus on nerve roots. Experimental models of nerve root compression in pigs are described. Rapid onset compression induces more edema than slow onset compression. Multiple levels of compression may increase substance P. Tumor necrosis factor (TNF) is identified as a key mediator of nerve dysfunction and pain by inducing axonal and myelin injury, increasing vascular permeability, and causing spontaneous electrical activity in nociceptors.