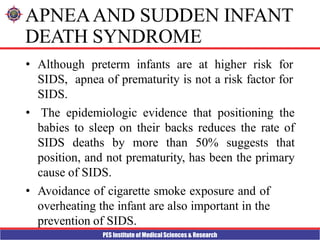
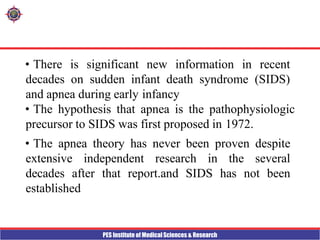
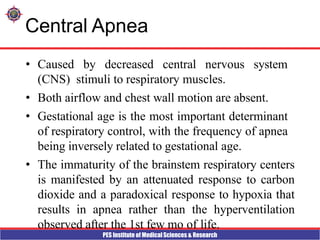
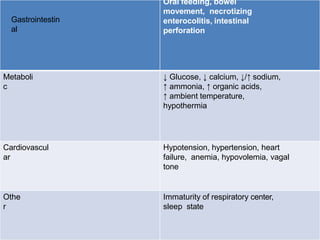
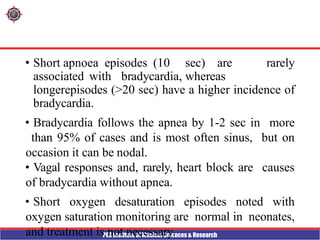
This document discusses apnea of prematurity, which is more common in preterm infants and involves cessation of breathing. It defines apnea and describes the different types - obstructive, central, and mixed. Potential causes are discussed along with clinical manifestations. Treatment typically involves cardiorespiratory monitoring, stimulation, caffeine/theophylline, CPAP, or doxapram. Prognosis is generally good unless apnea is severe and refractory. The document also discusses SIDS and notes that while preterm infants are at higher risk, apnea of prematurity itself is not a risk factor.








![PES Institute of Medical Sciences & Research
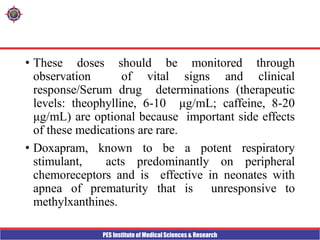
• Transfusion of packed red blood cells to reduce
the incidence of idiopathic apnea is reserved for
severely anemic infants.
• Nasal continuous positive airway pressure
(continuous positive airway pressure [CPAP], 3-5 cm
H2O) and high- flow humidification using nasal
cannula (1-2.5 L/min) are therapies for mixed or
obstructive apnea, but
CPAP is preferred because of its proven efficacy and
safety. The efficacy of CPAP is related to its ability to
splint the upper airway and prevent airway
obstruction.](https://image.slidesharecdn.com/neonatalapnea-230424034925-a8c06055/85/NEONATAL-APNEA-pptx-15-320.jpg)