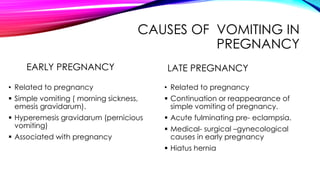
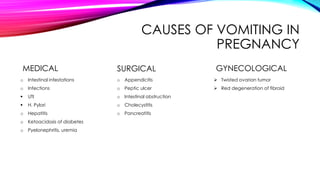
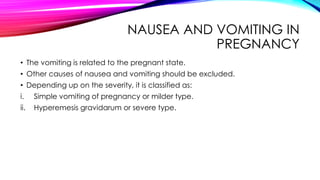
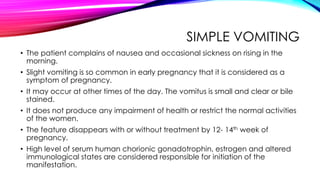
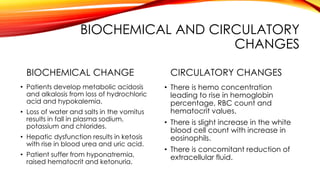
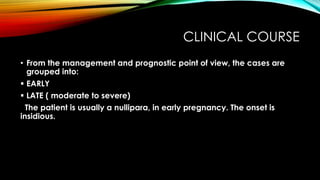
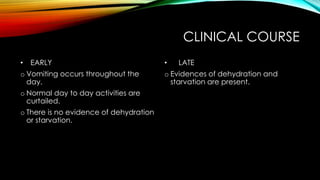
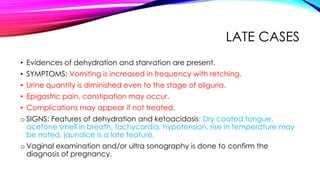
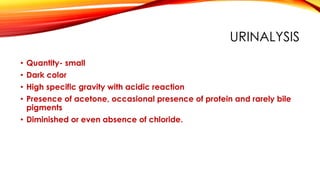
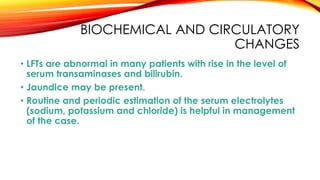
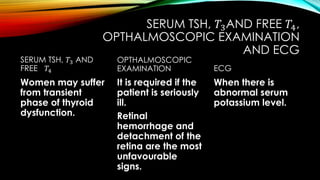
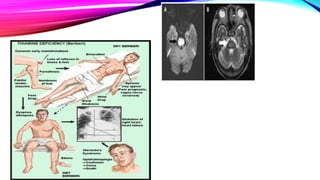
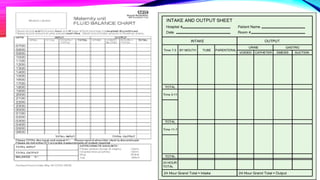
Nausea and vomiting during pregnancy, primarily attributed to hormonal changes, can range from mild morning sickness to severe hyperemesis gravidarum, which significantly impacts maternal health. Diagnosis involves confirming pregnancy and ruling out other medical conditions, with management focusing on hydration, antiemetics, and nutritional support. Complications may include dehydration, electrolyte imbalances, and risks to fetal health, necessitating careful monitoring and intervention.