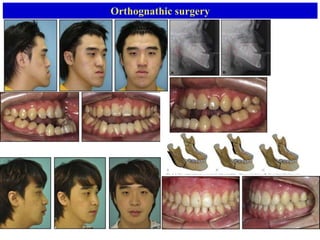
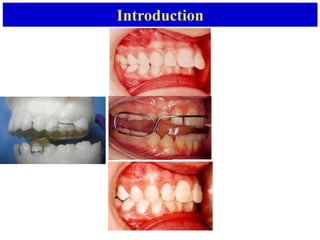
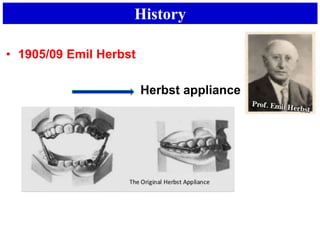
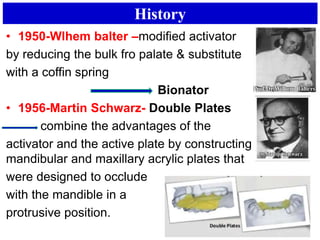
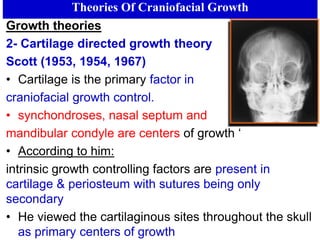
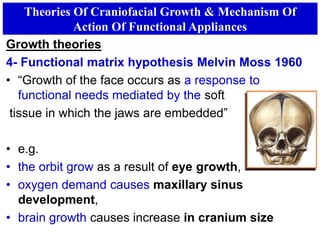
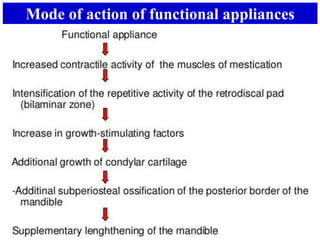
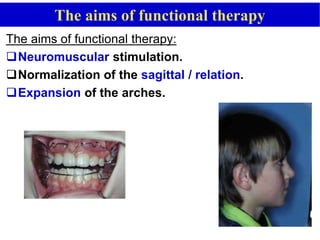
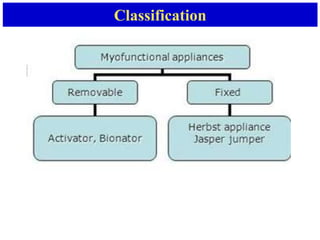
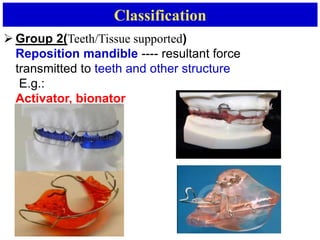
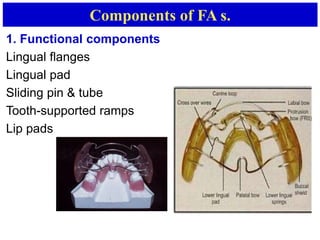
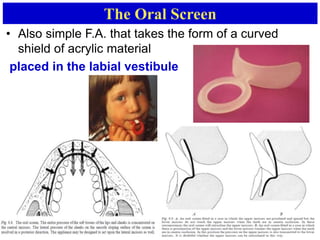
This document discusses orthodontic appliances called functional or myofunctional appliances. It begins with definitions of these appliances as removable or fixed devices that change the position of the mandible to transmit forces from stretched muscles and soft tissues to the dentition and skeletal structures. The document then covers the history of functional appliances dating back to the late 1800s, theories of craniofacial growth, how these appliances work to modify growth, common types including the activator and bionator, components, and clinical management considerations. The overall purpose of functional appliances is to correct malocclusions like Class II issues through modifying growth and altering the soft tissue environment.