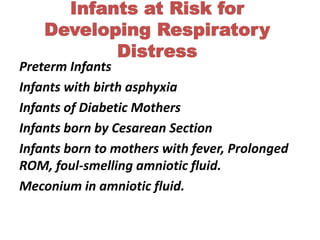
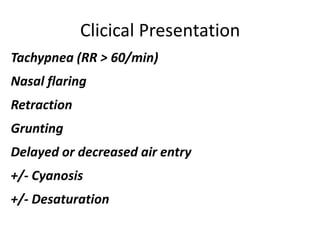
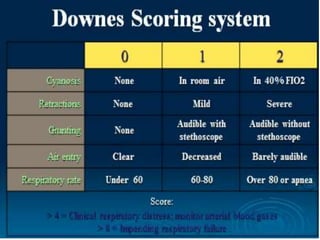
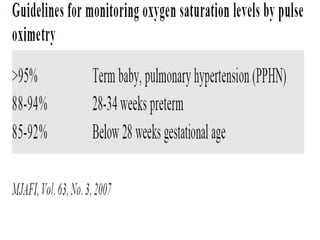
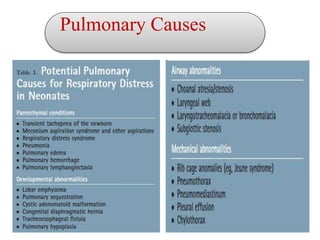
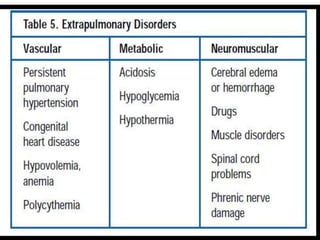
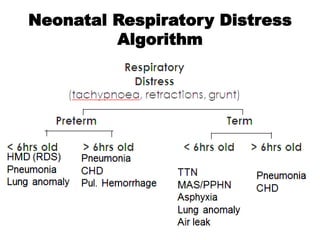
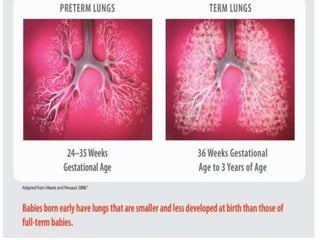
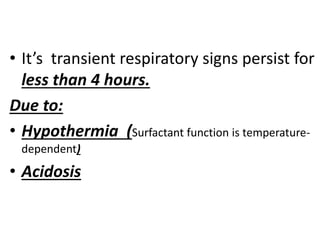
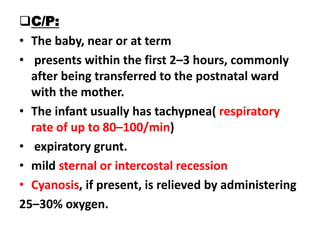
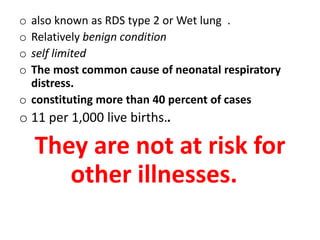
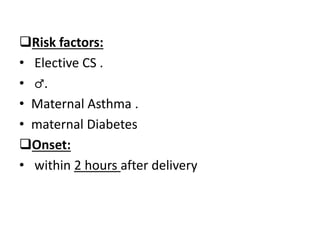
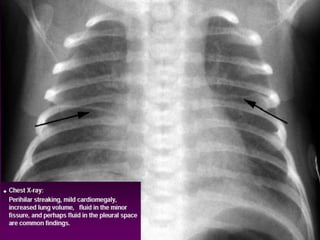
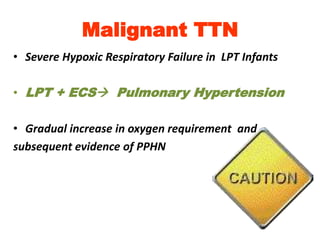
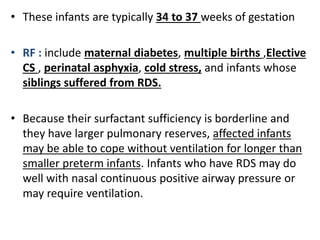
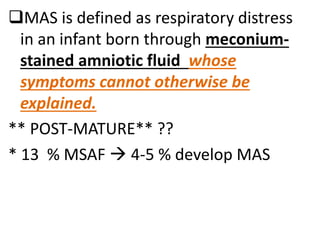
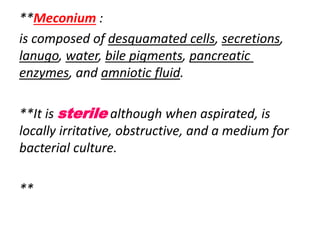
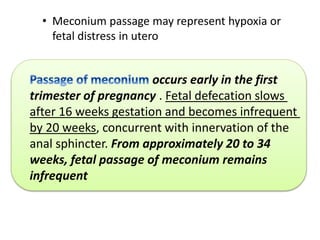
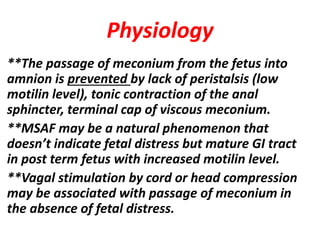
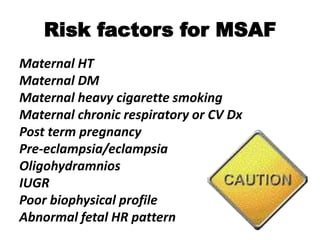
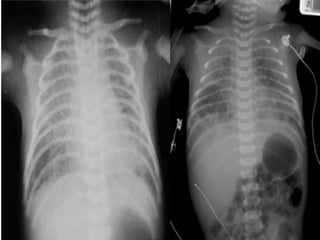
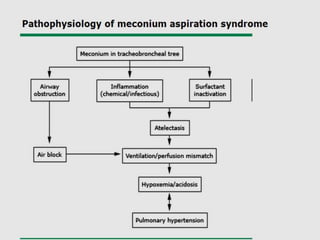
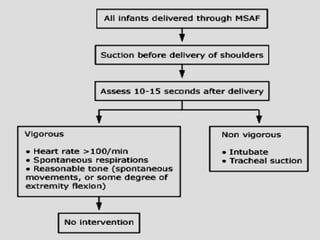
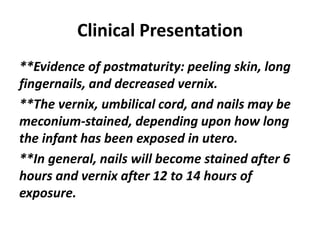
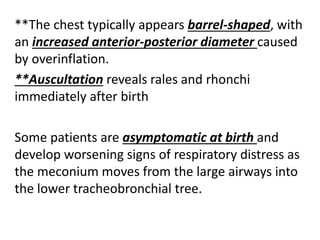
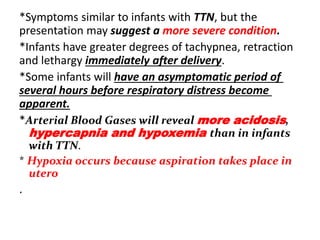
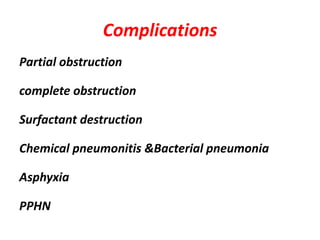
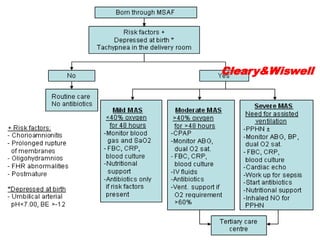
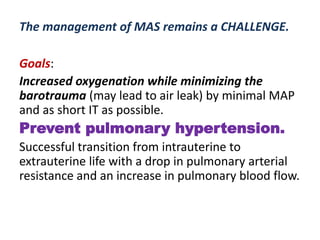
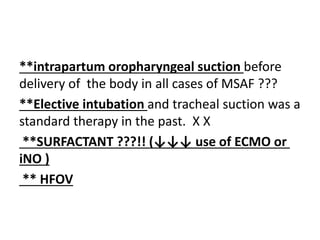
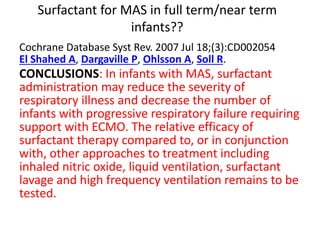
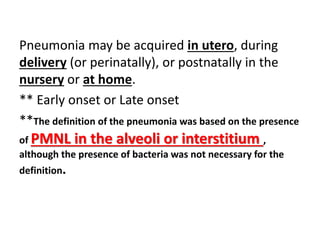
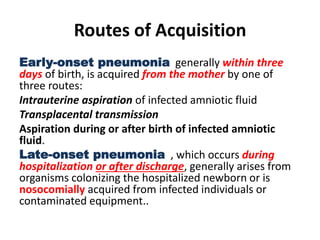
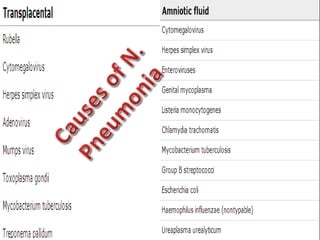
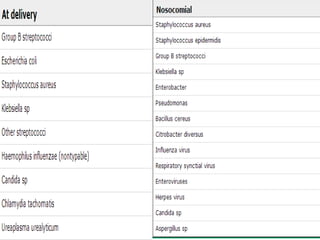
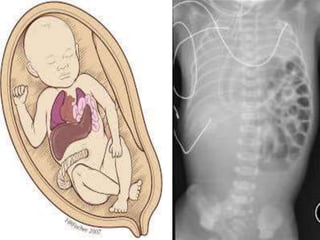
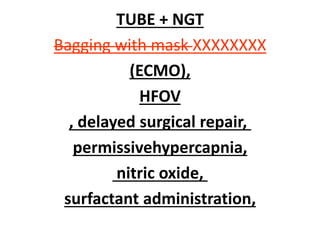
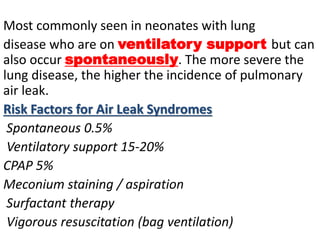
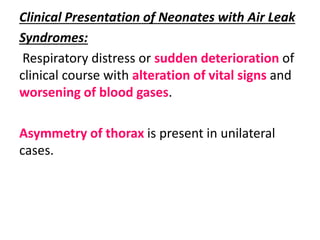
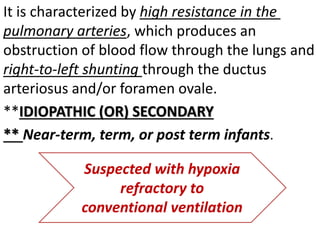
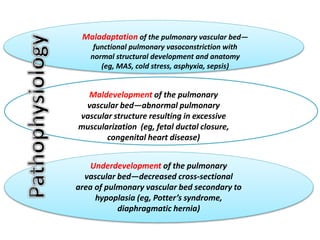
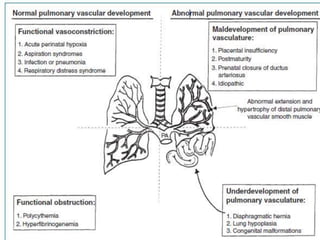
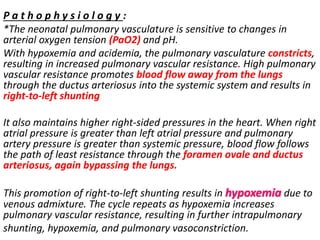
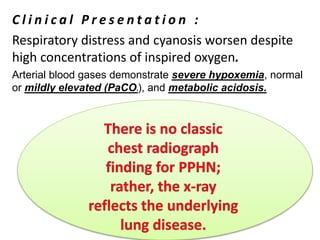
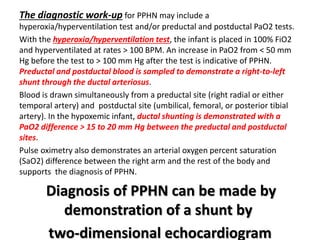
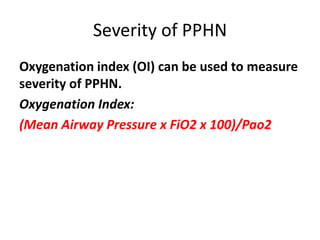
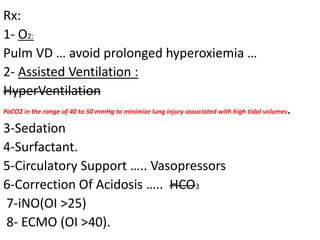
This document discusses respiratory distress in term and near-term infants. It outlines several common causes of respiratory distress including transient tachypnea of the newborn (TTN), respiratory distress syndrome (RDS), meconium aspiration syndrome (MAS), pneumonia, congenital diaphragmatic hernia (CDH), pulmonary air leak syndromes, and persistent pulmonary hypertension of the newborn (PPHN). For each cause, it describes risk factors, clinical presentation, pathophysiology, diagnosis, and management. The goal of management is to support oxygenation and ventilation while minimizing lung injury until the underlying condition resolves.