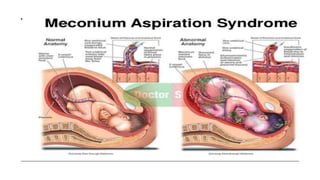
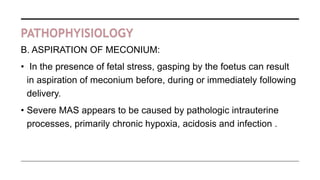
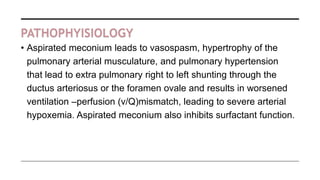
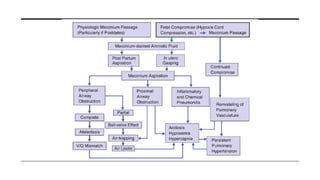
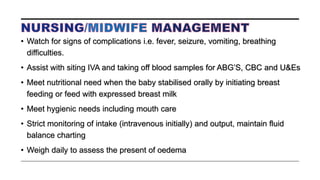
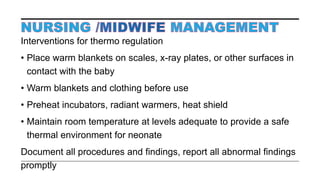
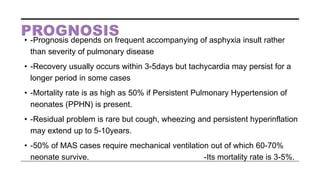
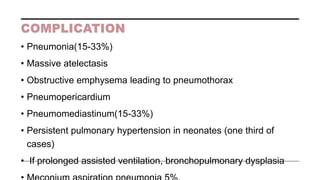
Meconium aspiration syndrome (MAS) occurs when meconium, the first stool of infants, is aspirated into the lungs before, during, or immediately after birth, often due to fetal distress. It can cause respiratory distress, lung damage, or even death in newborns. Risk factors include postmaturity, fetal hypoxia, and meconium-stained amniotic fluid. Treatment involves suctioning the airways, oxygen therapy, antibiotics, and supportive care. Outcomes depend on severity but may include complications like pneumonia. Preventive measures focus on monitoring high-risk pregnancies and deliveries to identify fetal distress early.