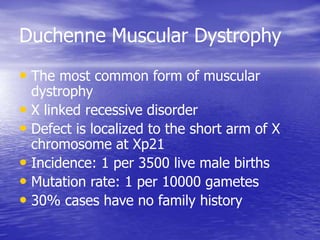
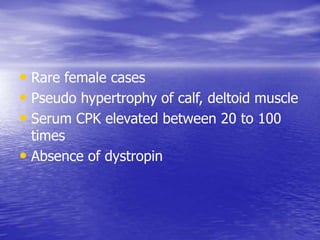
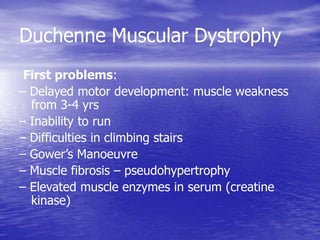
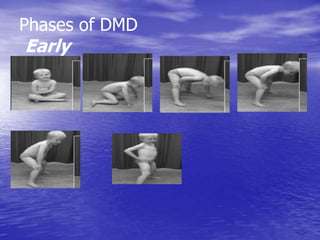
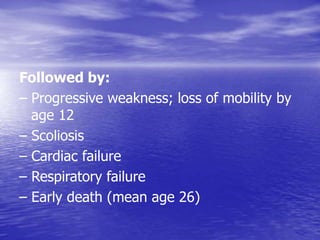
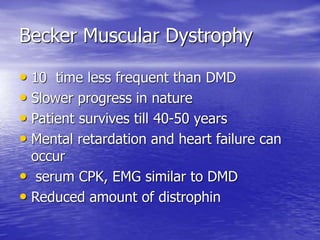
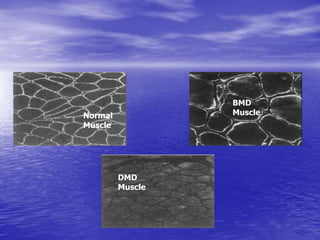
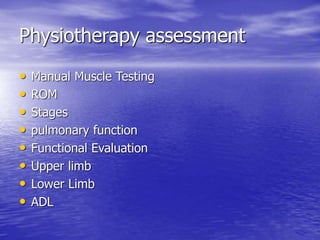
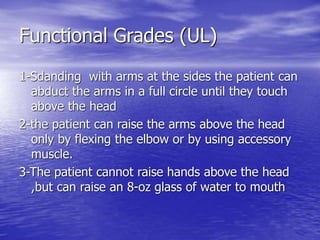
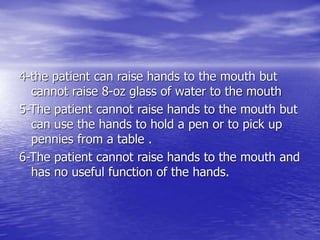
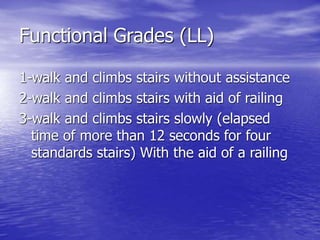
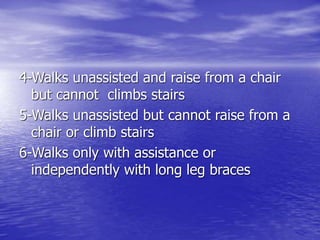
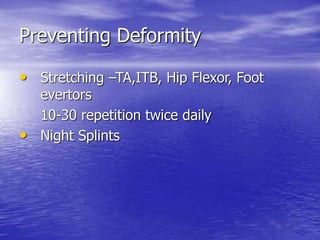
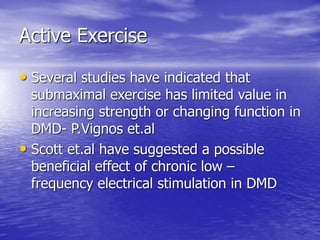
This document summarizes muscular dystrophy, focusing on Duchenne muscular dystrophy (DMD). It defines DMD as the most common and severe form of muscular dystrophy, caused by an absence of the protein dystrophin. The document outlines the signs and symptoms of DMD including muscle weakness, loss of ambulation by age 12, and early death typically around age 26. Physical therapy for DMD aims to prolong functional ability, prevent deformities like scoliosis, and facilitate family support through the progression of the disease.