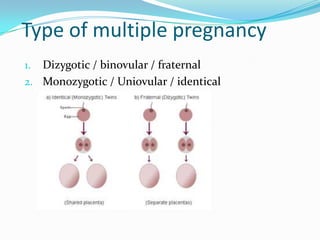
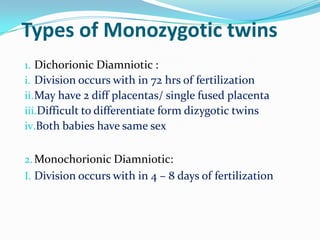
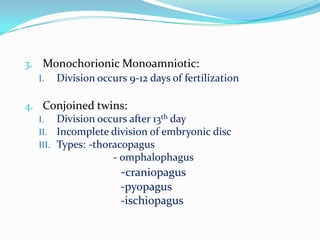
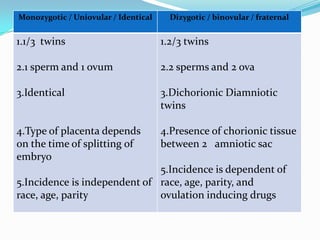
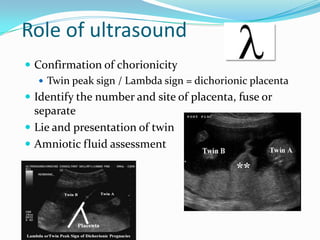
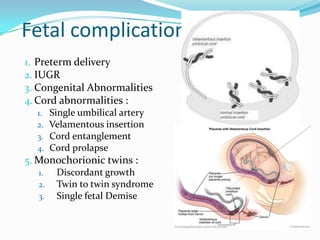
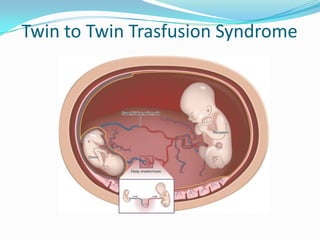
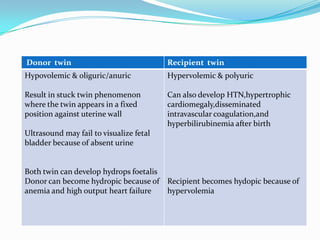
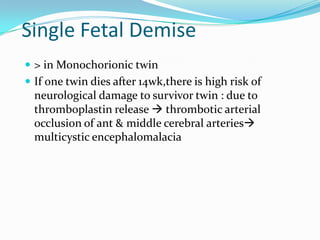
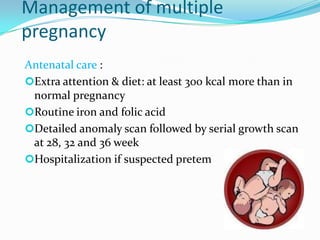
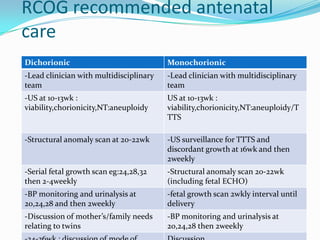
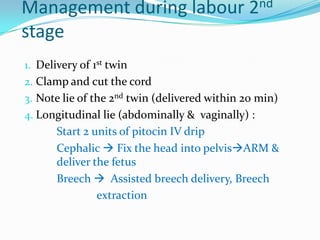
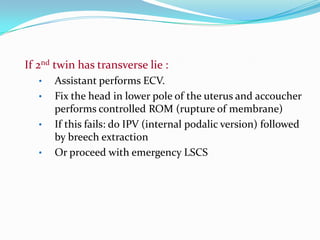
This document discusses multiple pregnancies, specifically twins. It defines twins as the simultaneous development of more than one fetus in the uterus. The types of twins are discussed, including dizygotic/fraternal twins which develop from two separate eggs and monozygotic/identical twins which develop from one egg. The risks and complications associated with multiple pregnancies are summarized for both the mother and fetuses. The document concludes with describing the recommended management and care during antenatal, delivery, and postnatal periods for multiple pregnancies.