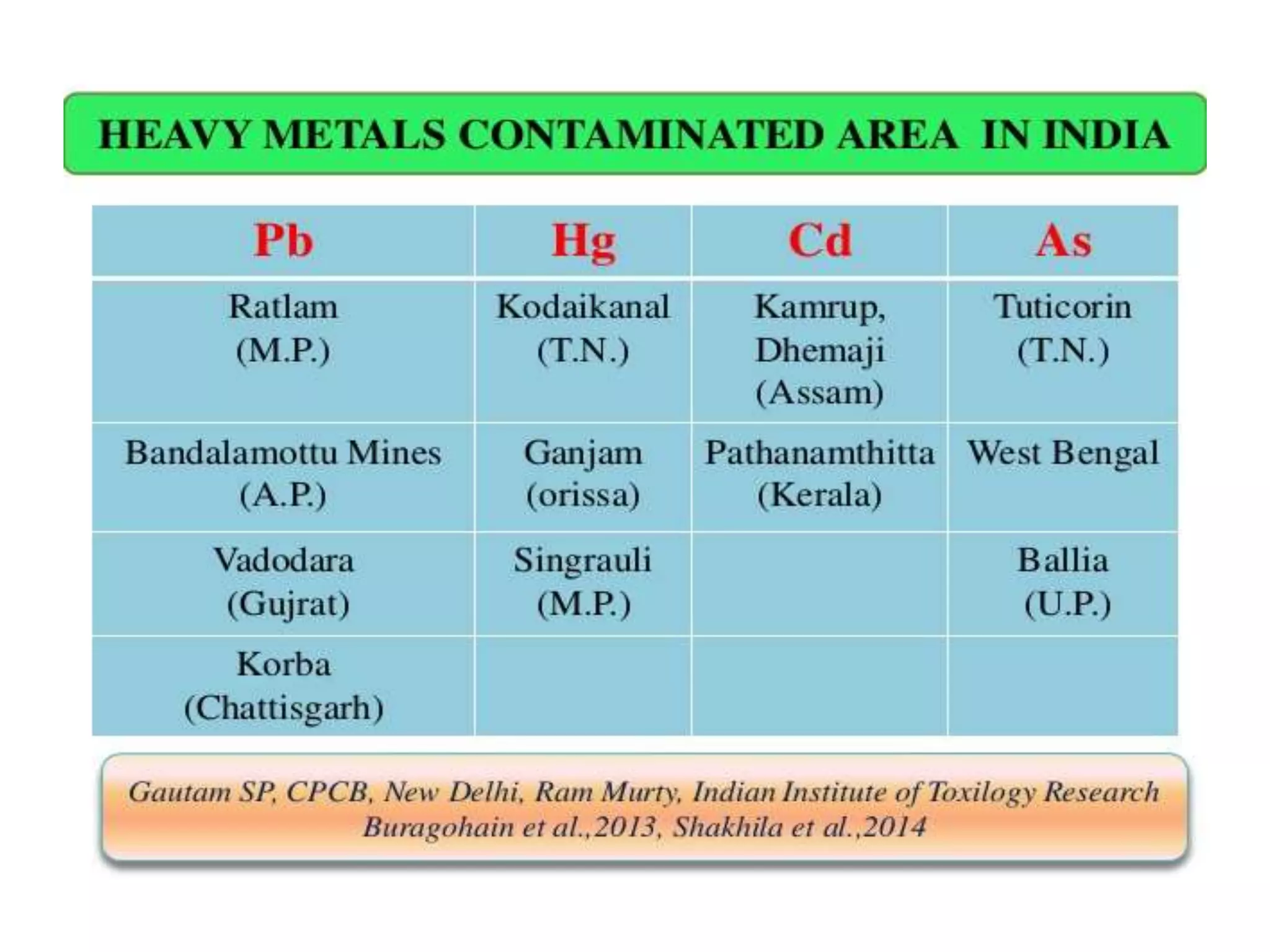
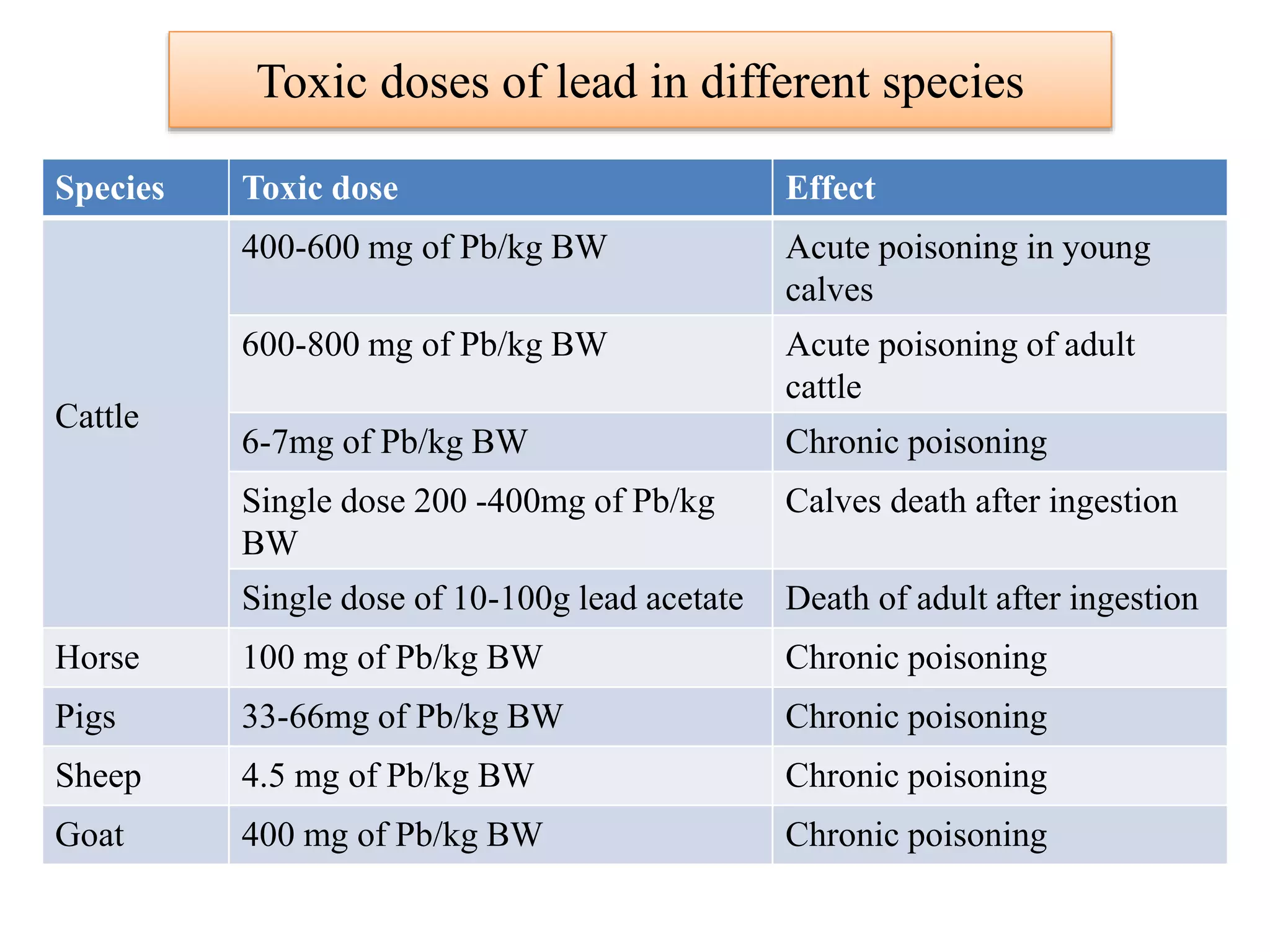
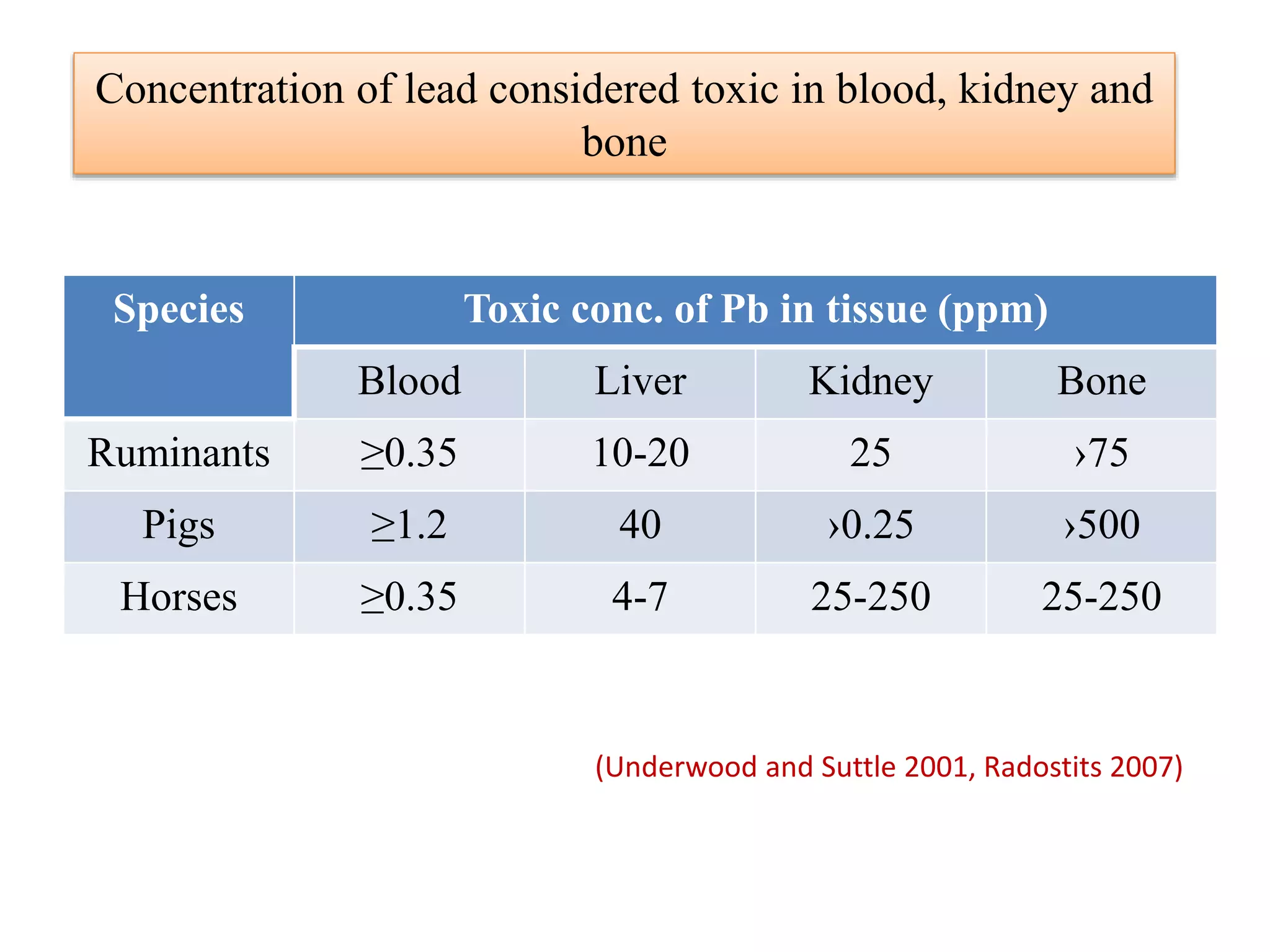
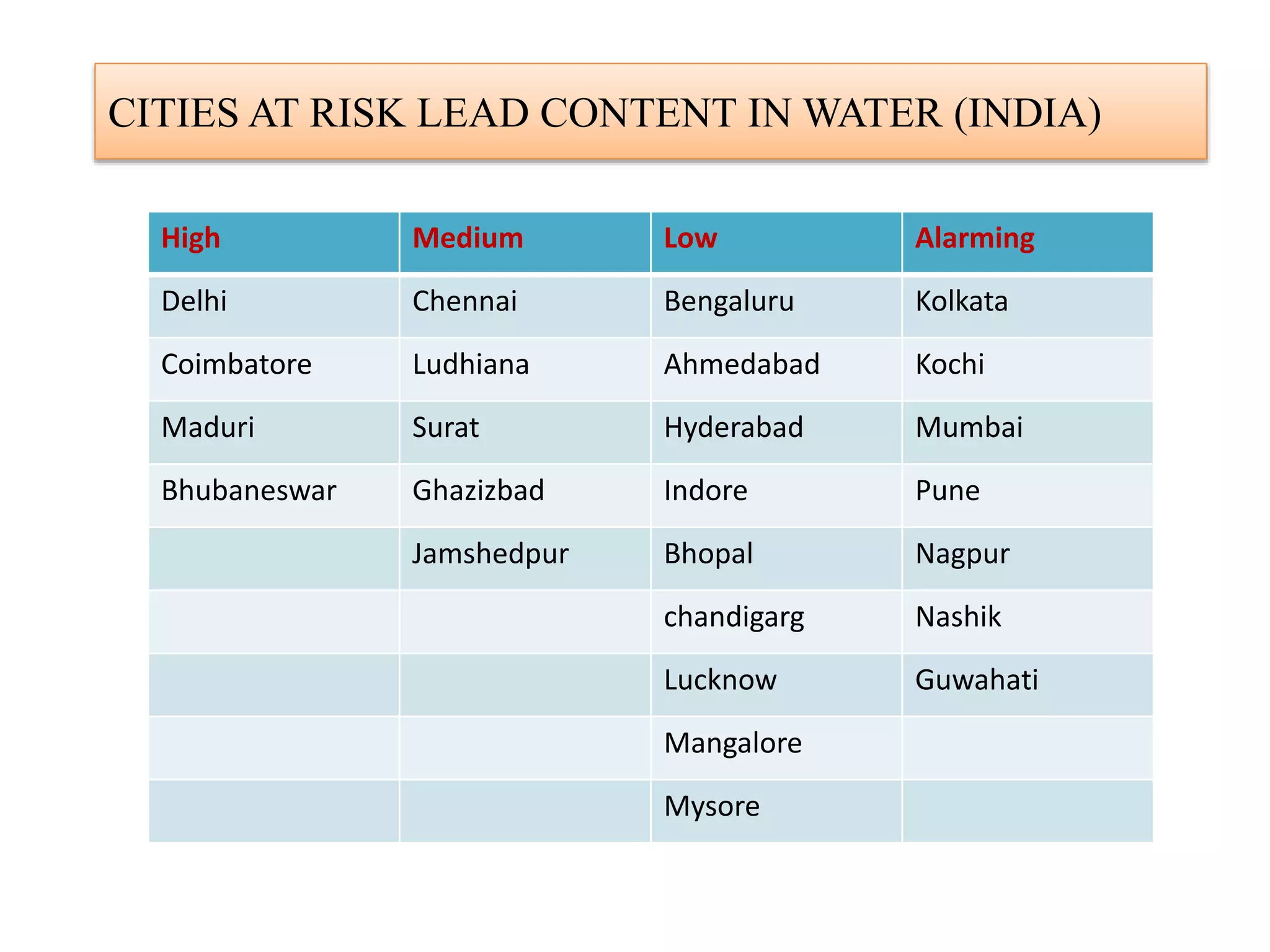
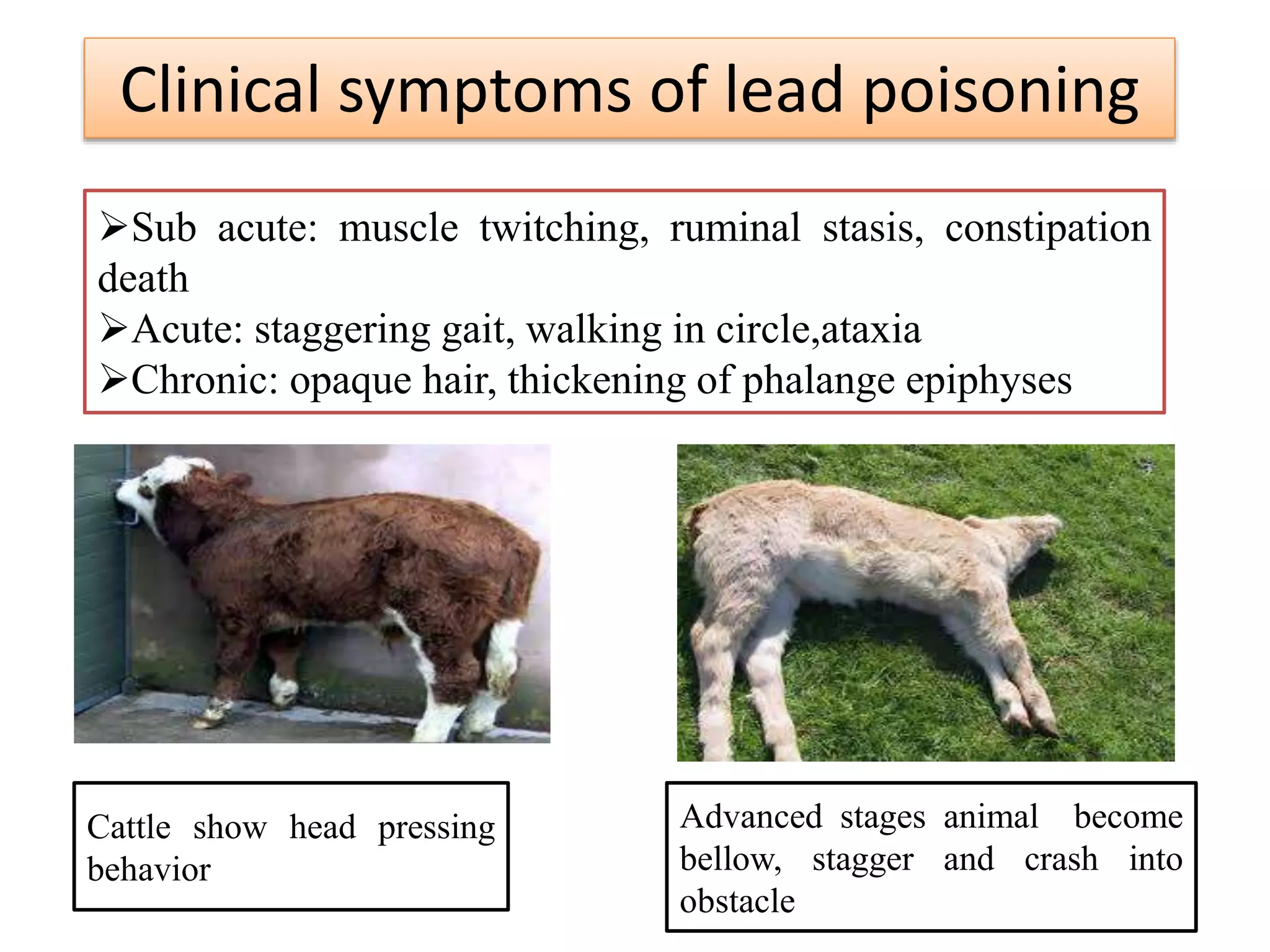
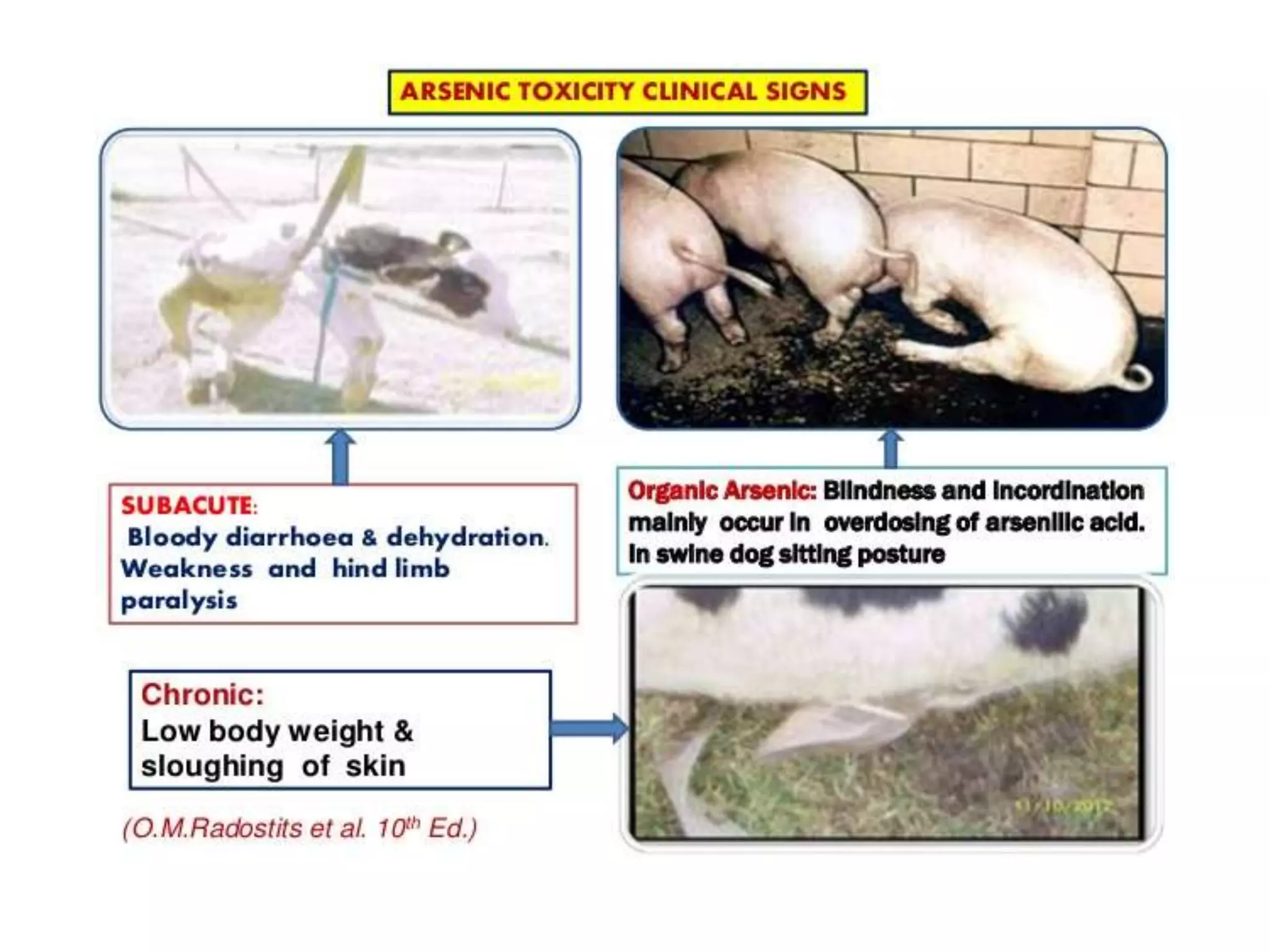
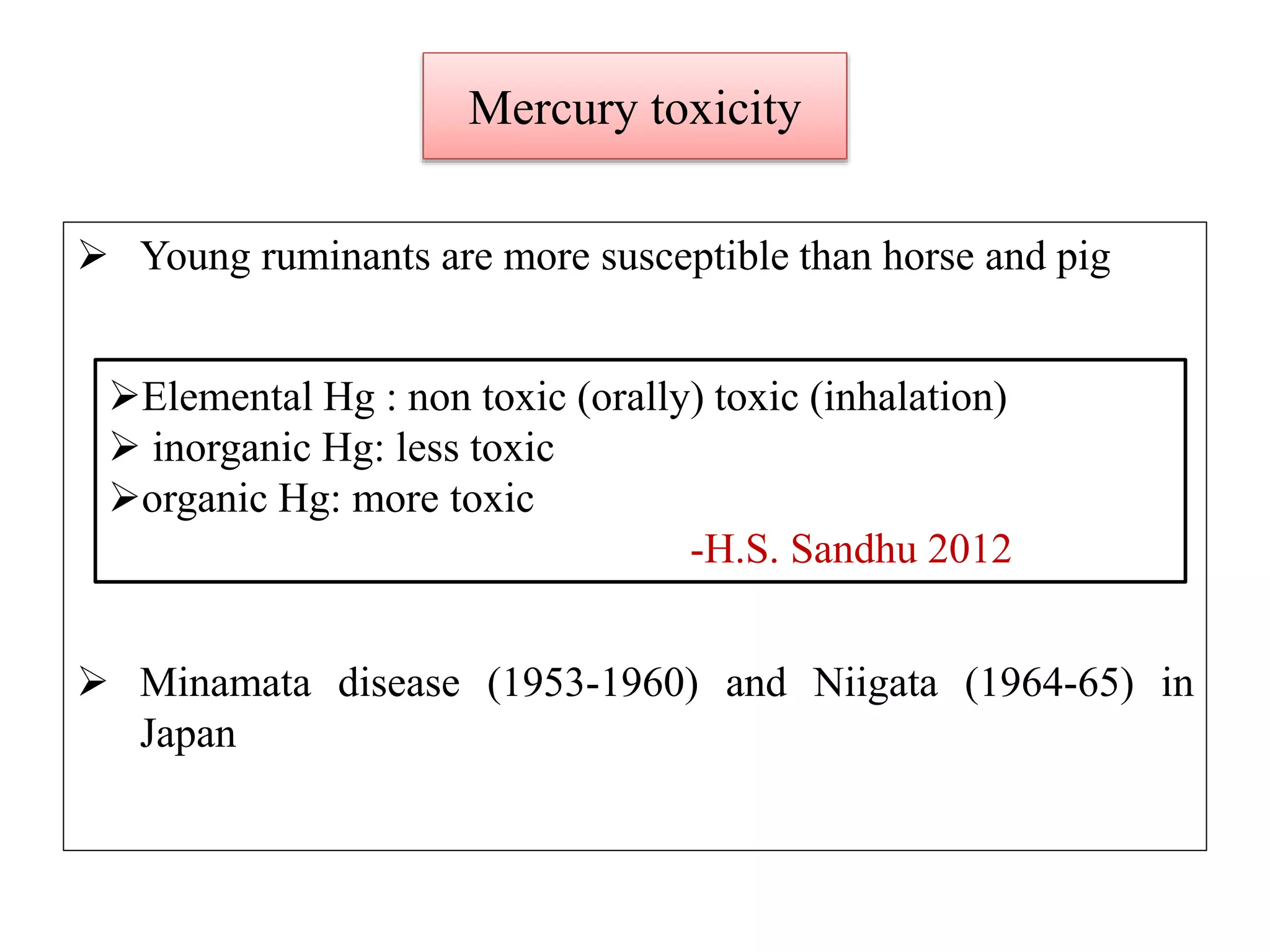
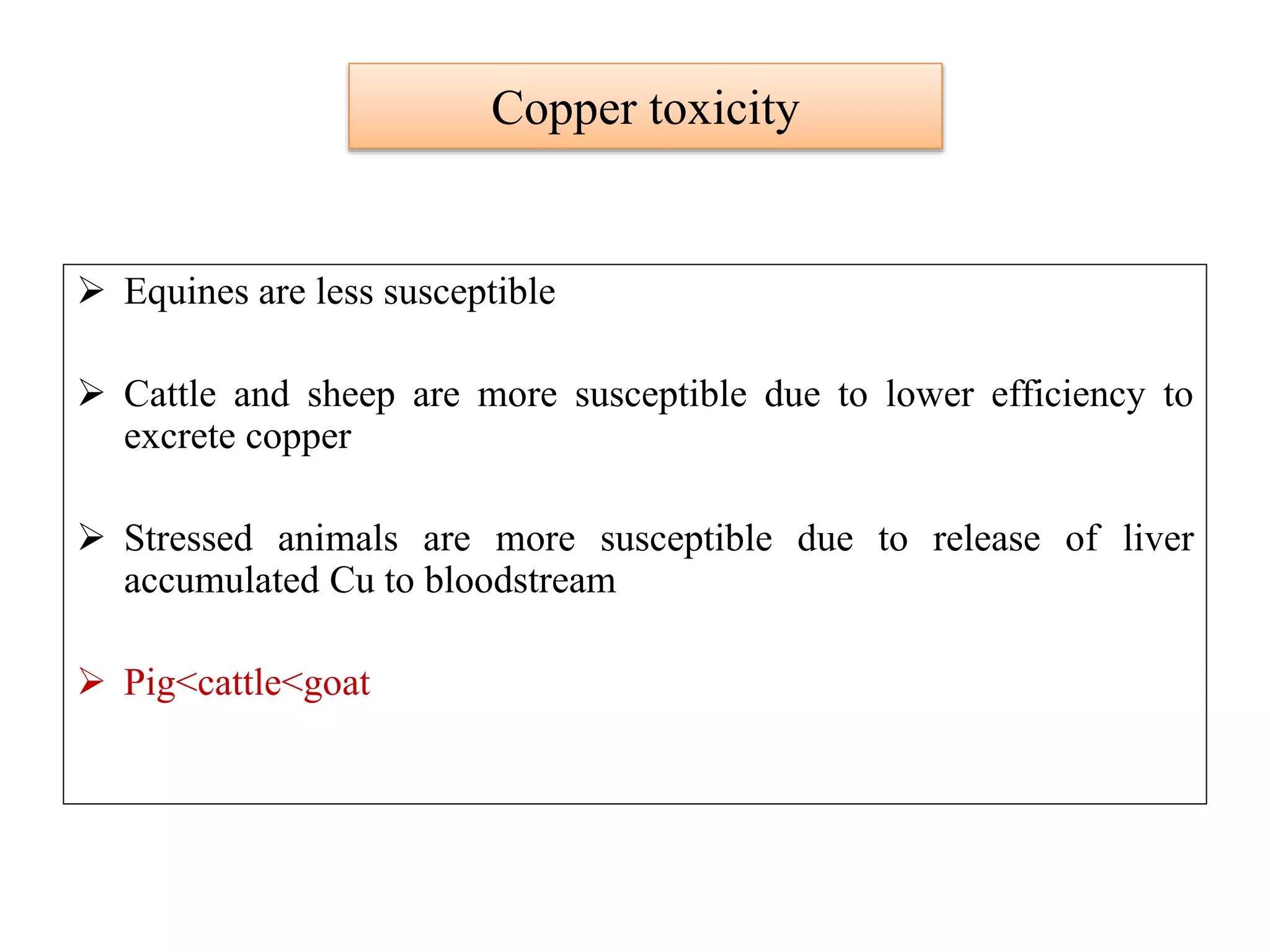
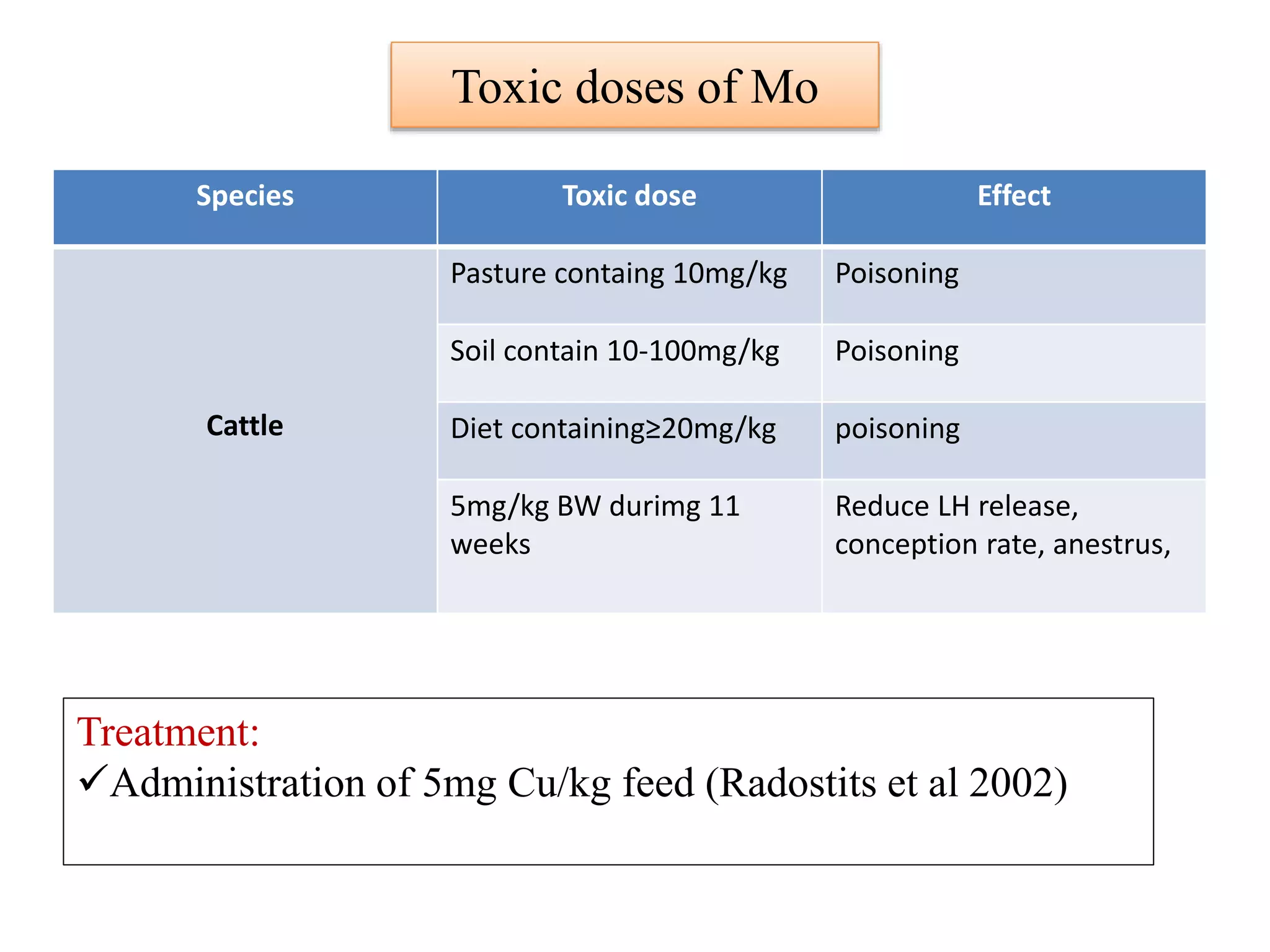
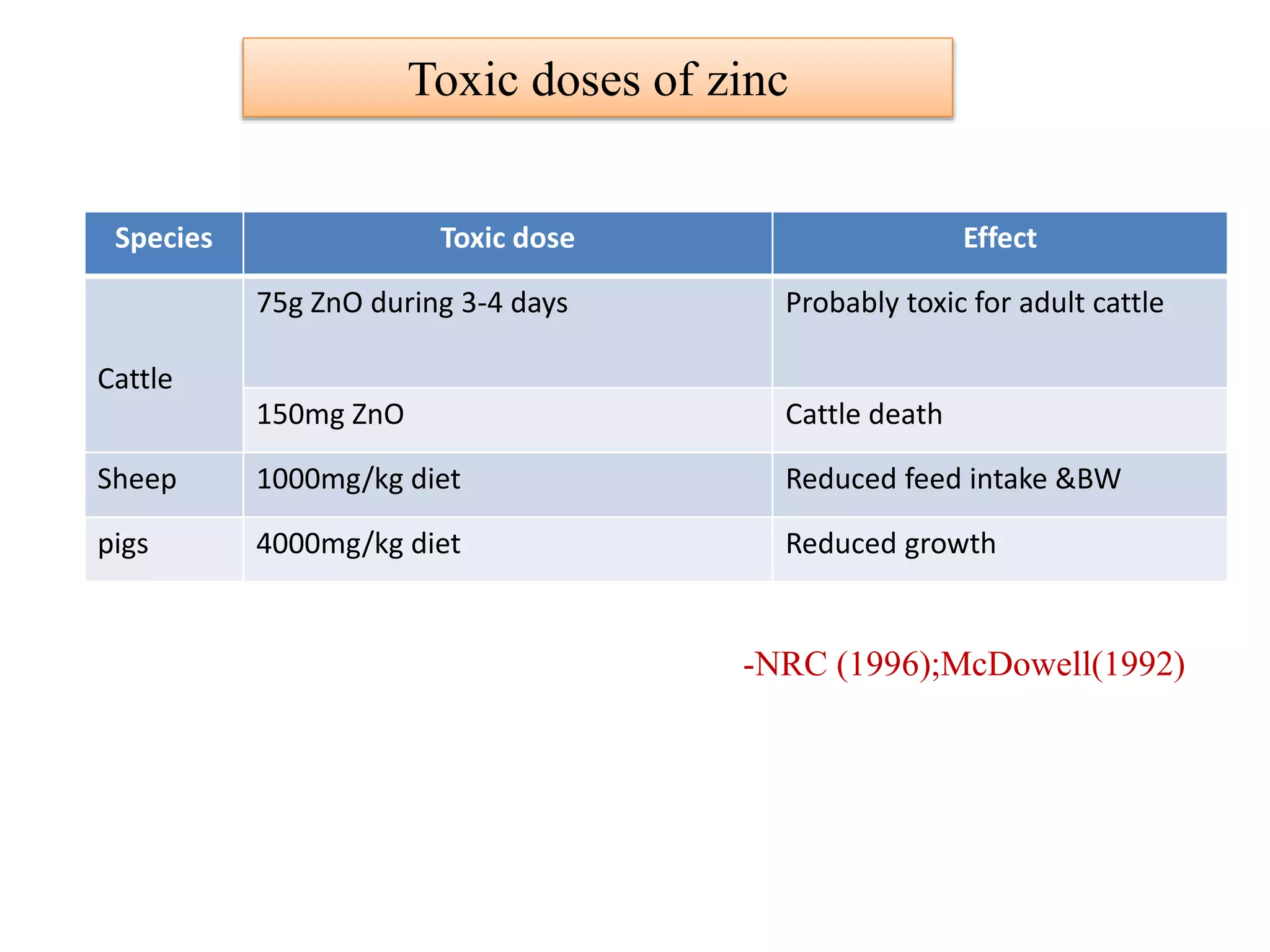
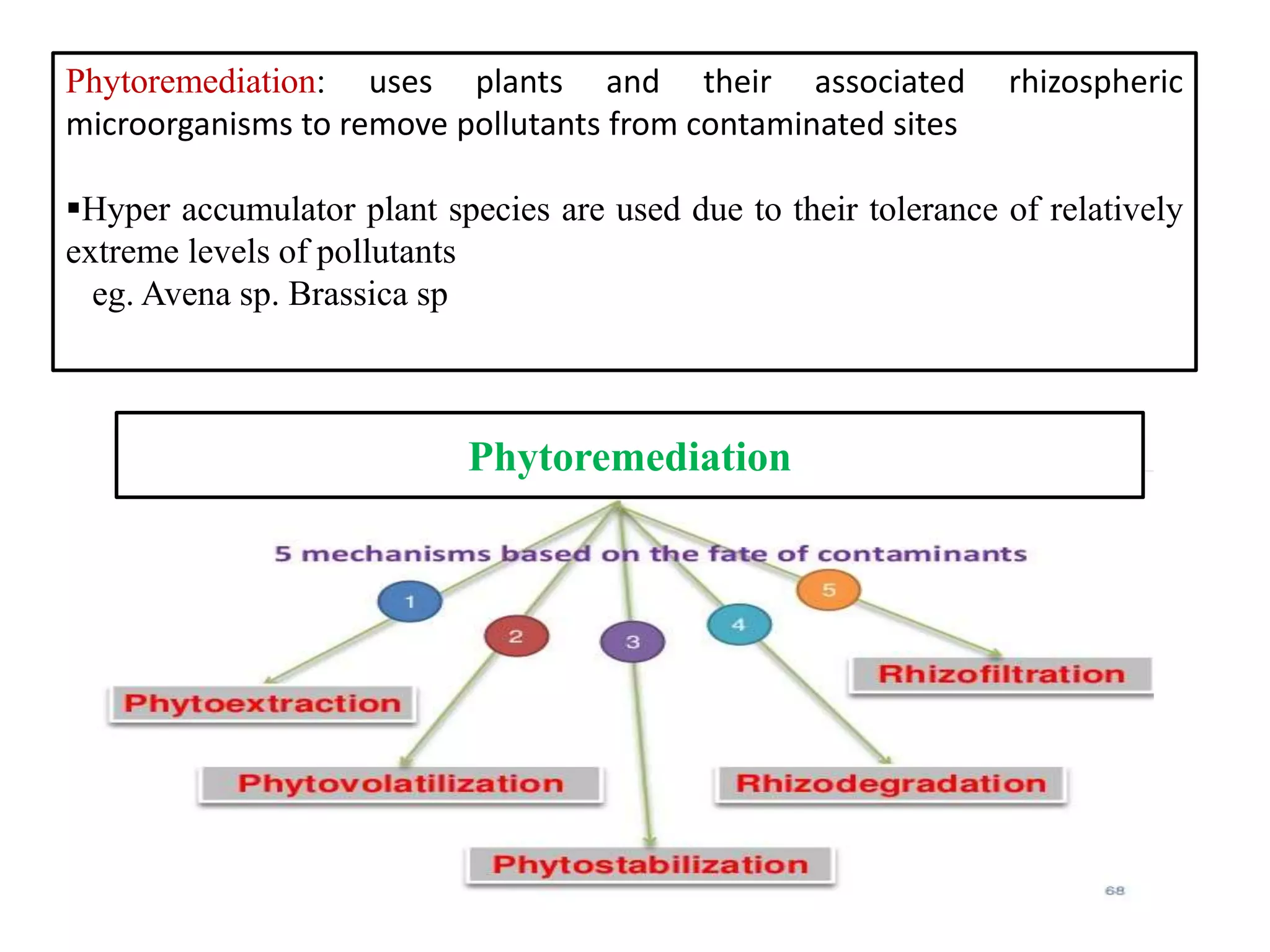
This document discusses mineral toxicity in livestock, including sources, clinical signs, and treatment. It covers the toxicity of various minerals such as lead, arsenic, mercury, cadmium, selenium, copper, molybdenum, zinc, fluorine, and manganese. For each mineral, it provides the toxic doses for different livestock species and describes the associated clinical symptoms and recommended treatment approaches. It also discusses general principles for managing mineral toxicity, including prevention of further absorption, elimination from circulation, and inactivation or decontamination. Bioremediation techniques using microbes and plants are mentioned for attenuating environmental pollutants.