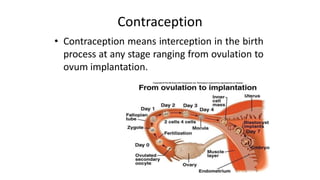
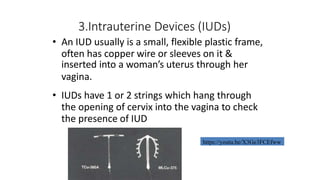
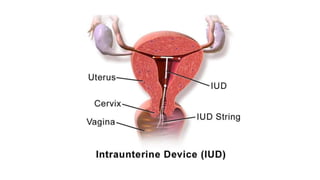
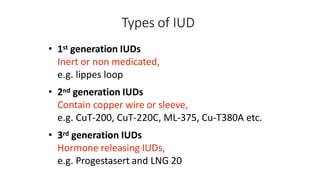
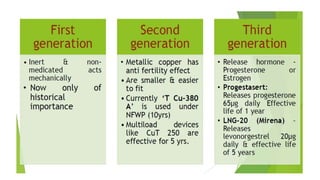
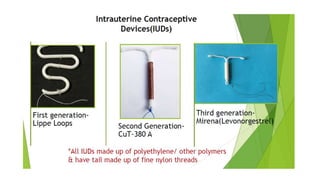
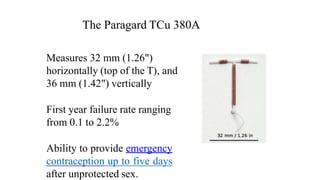
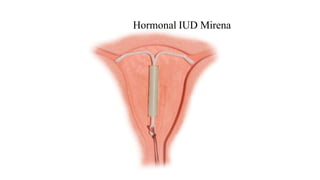
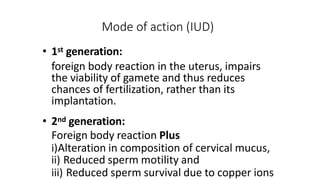
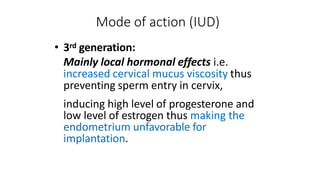
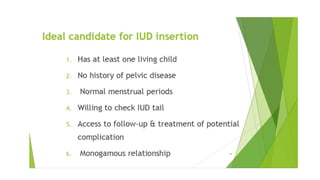
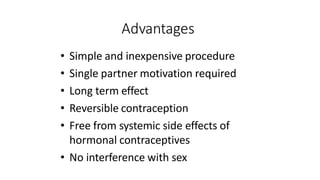
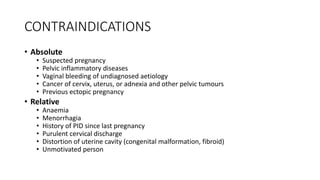
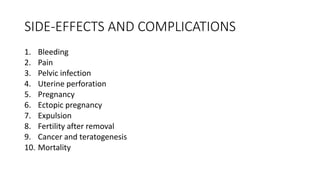
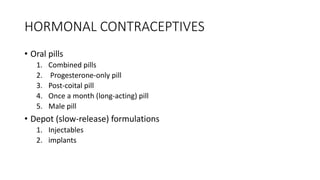
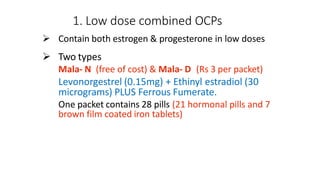
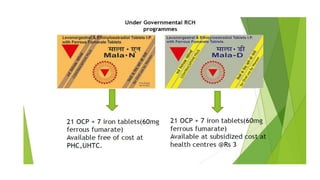
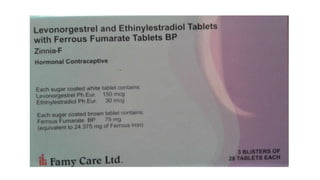
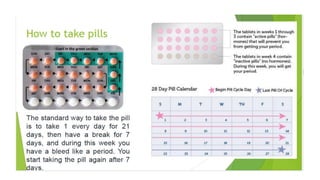
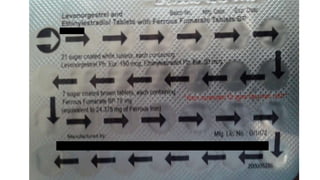
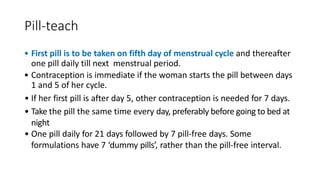
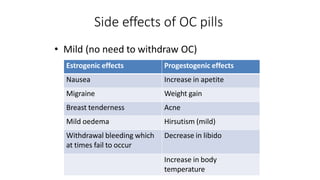
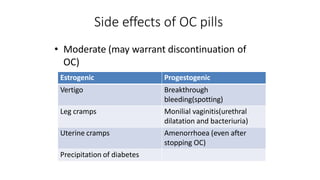
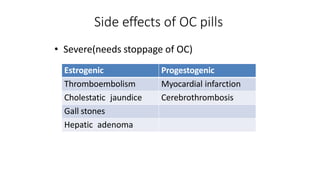
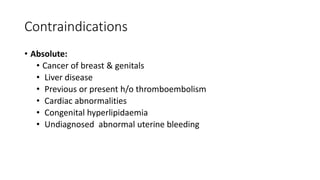
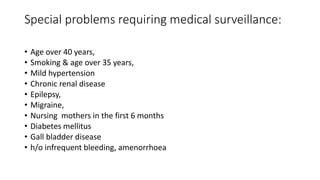
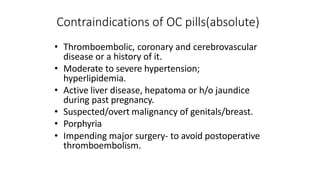
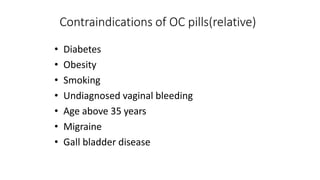
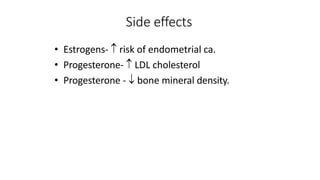
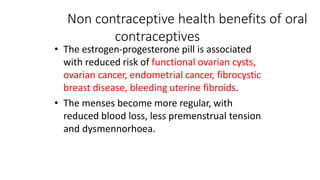
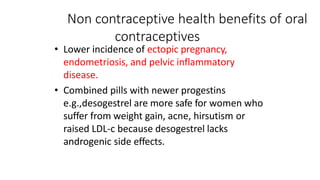
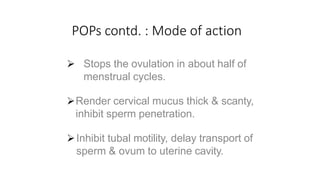
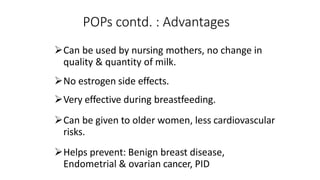
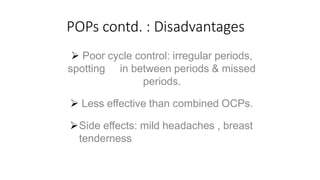
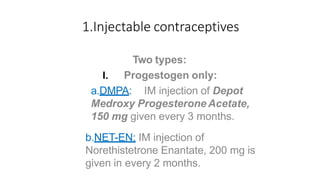
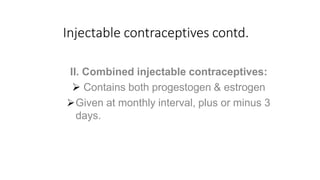
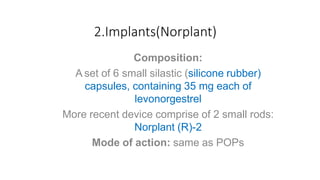
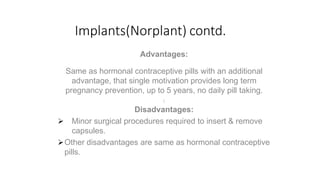
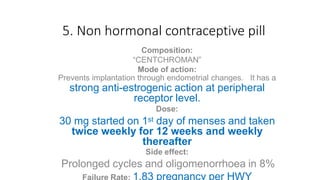
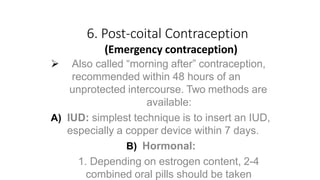
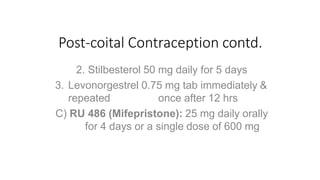
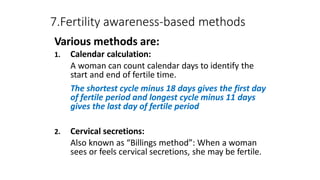
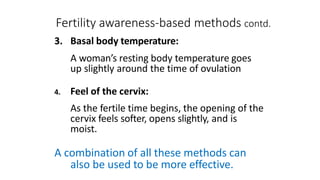
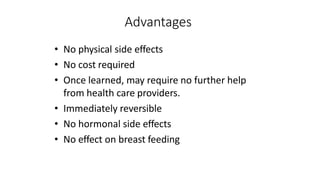
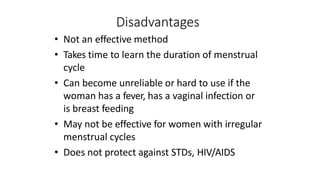
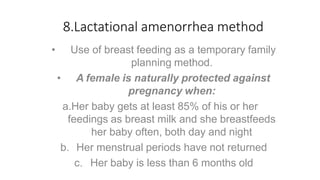
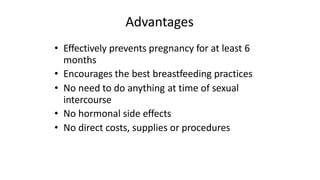
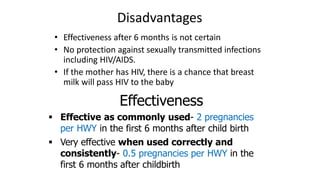
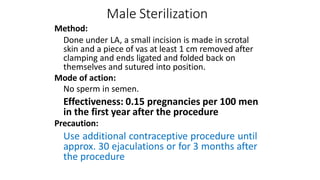
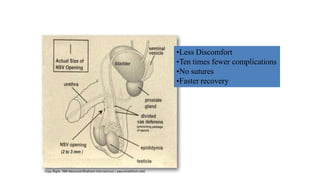
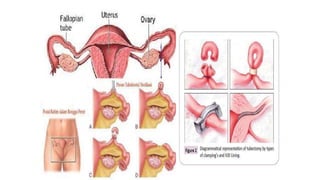
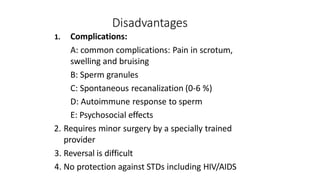
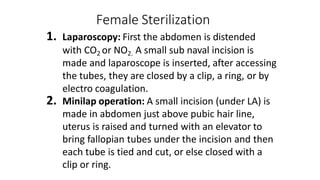
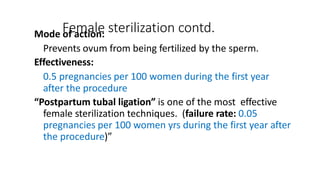
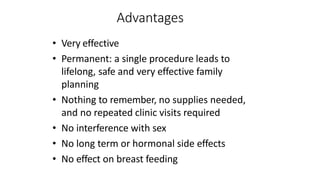
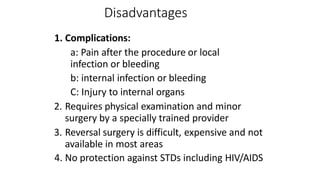
The document describes various methods of contraception, including temporary and permanent options. Temporary methods discussed include barrier methods like condoms, vaginal methods like spermicides and diaphragms, intrauterine devices (IUDs), and hormonal methods like oral contraceptive pills and injectables. Permanent methods discussed are male and female sterilization. The advantages, disadvantages, effectiveness, and other details are provided for many of the discussed contraception methods.