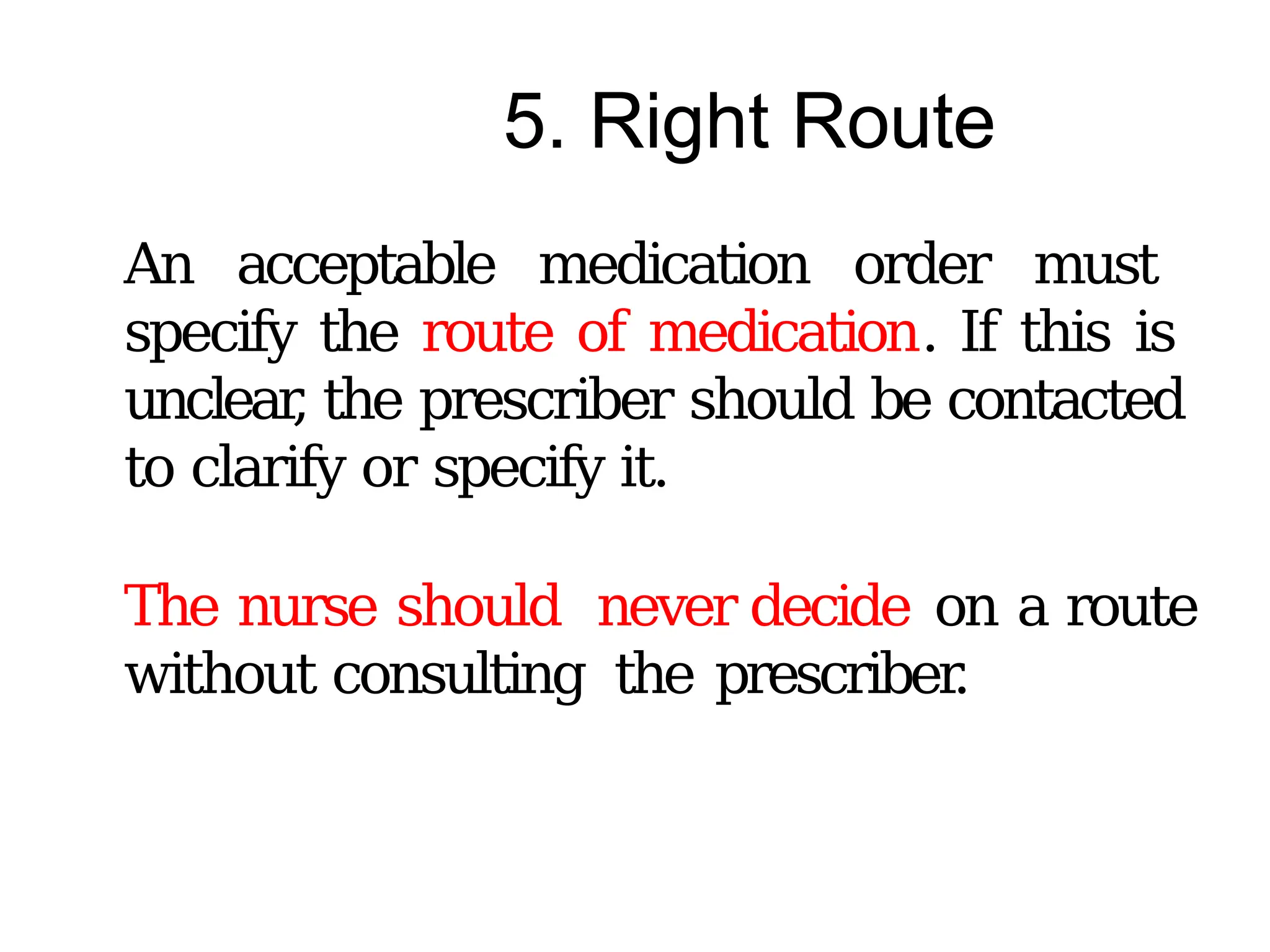
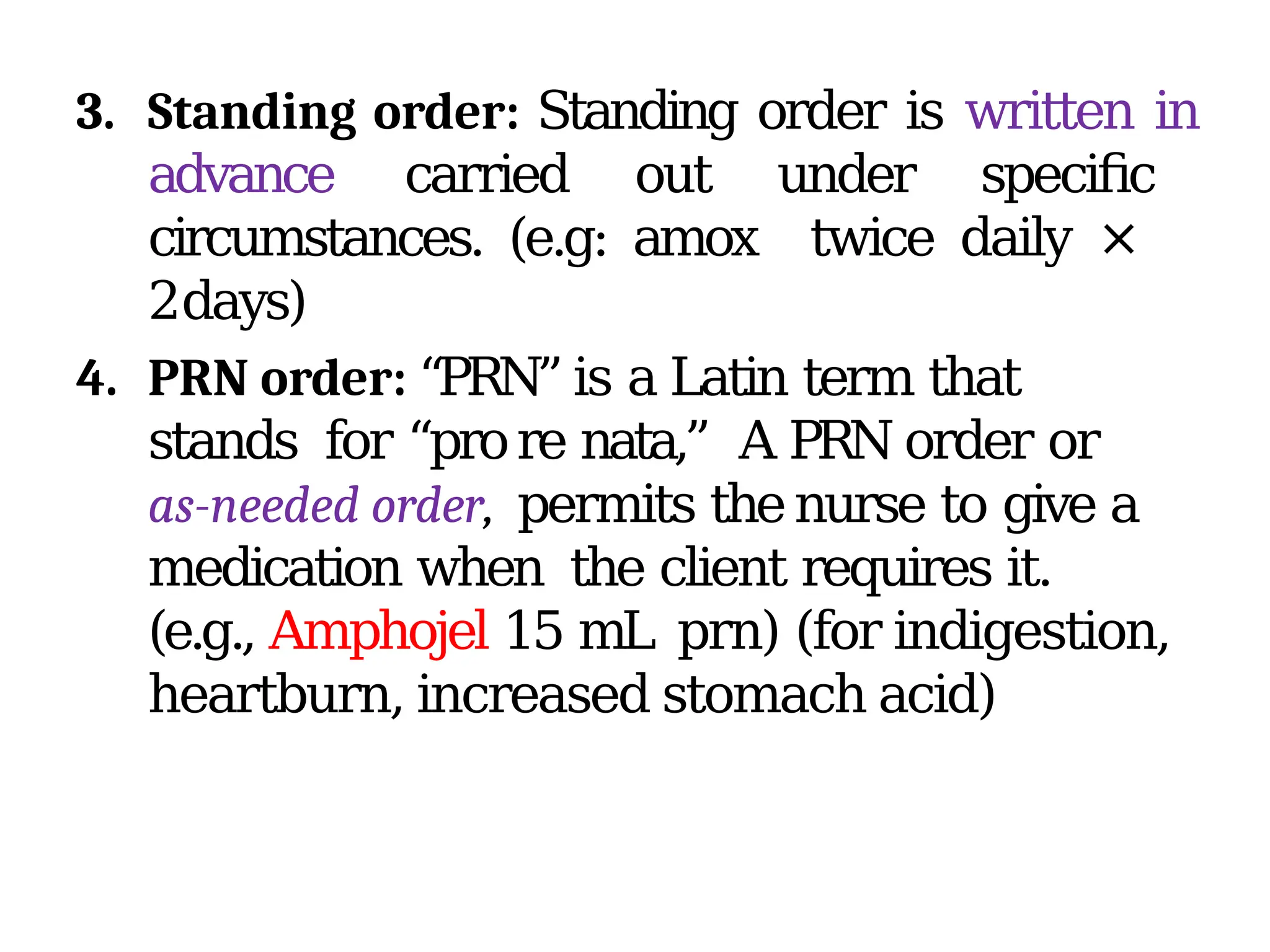
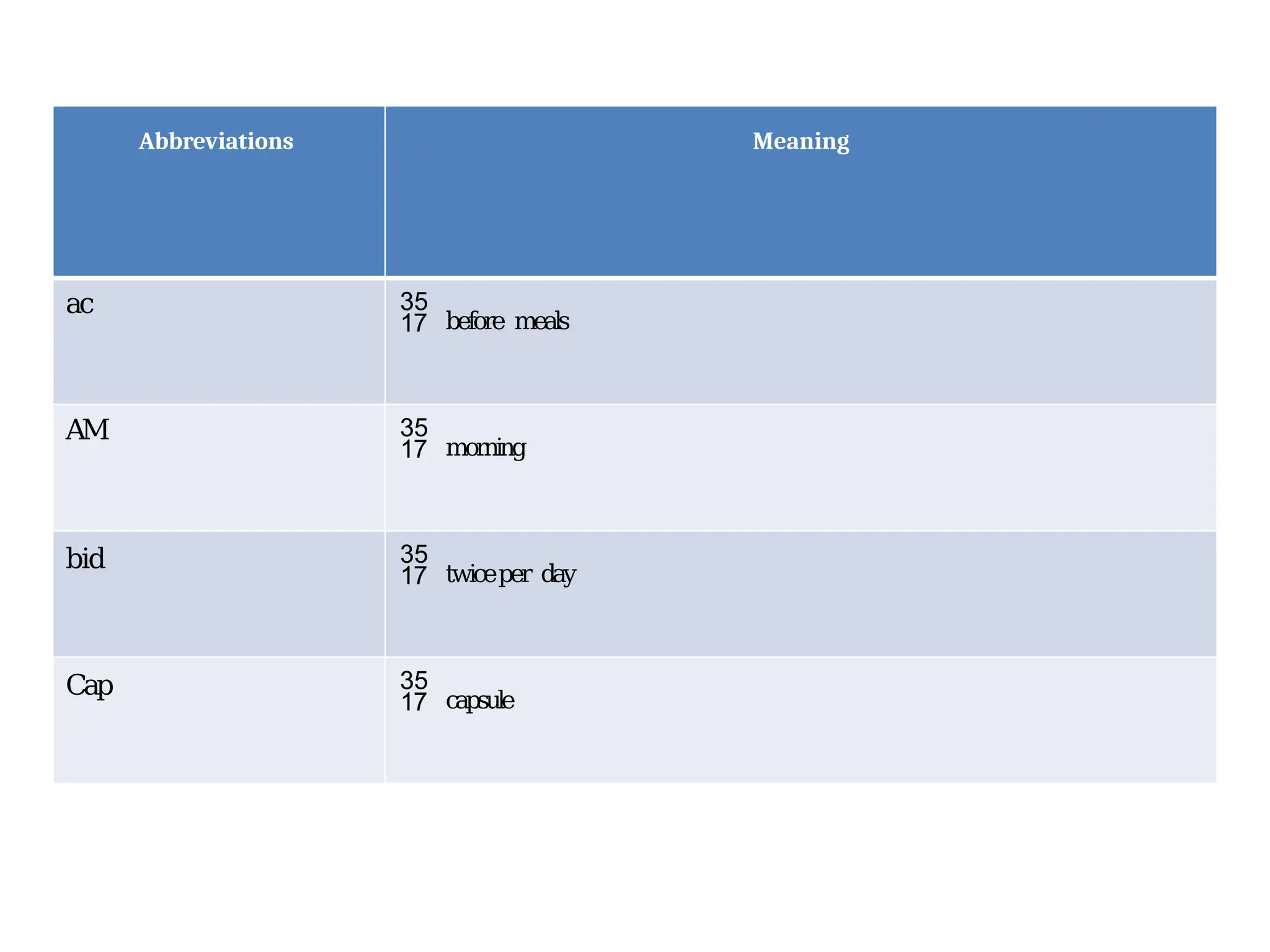
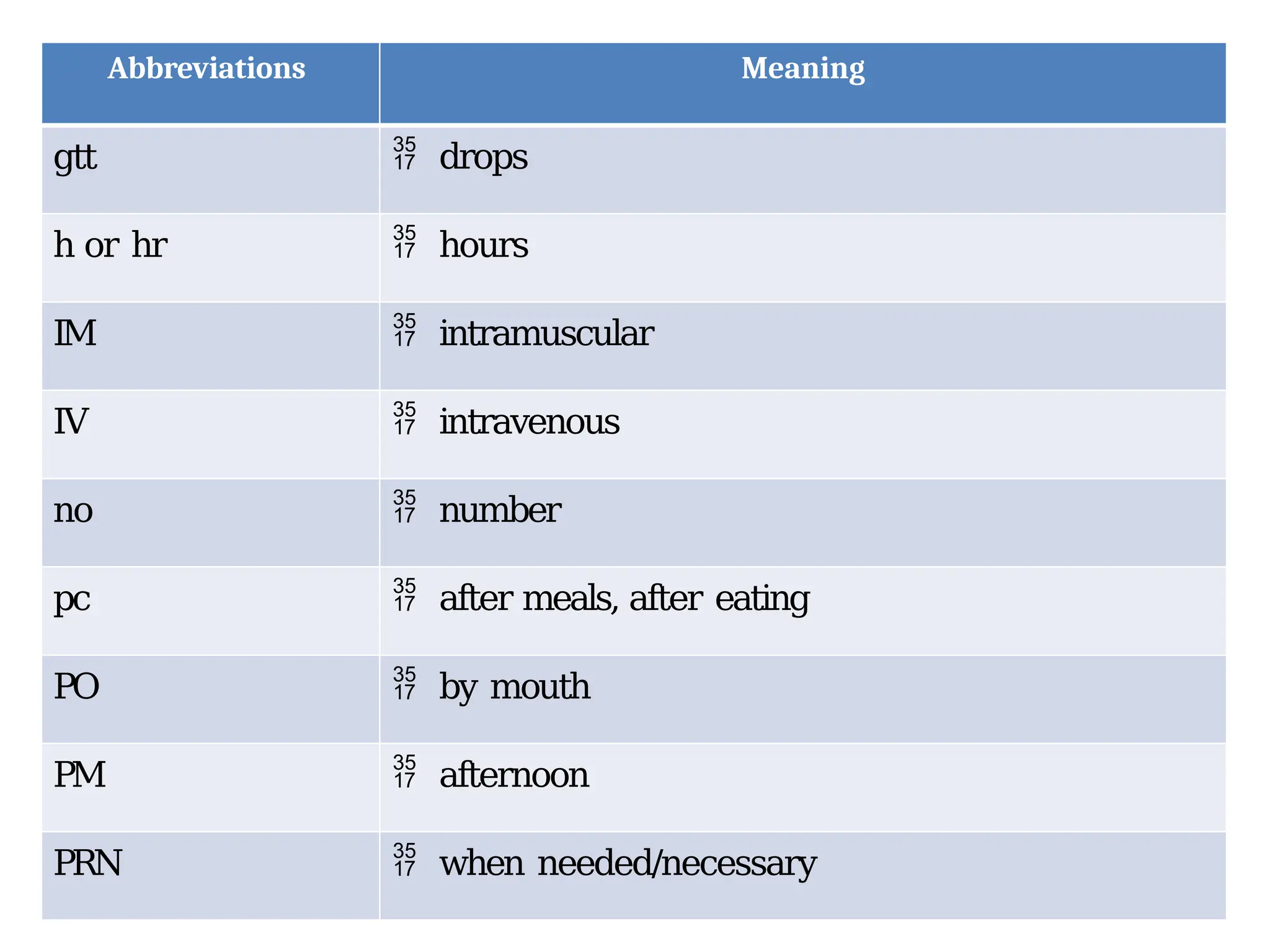
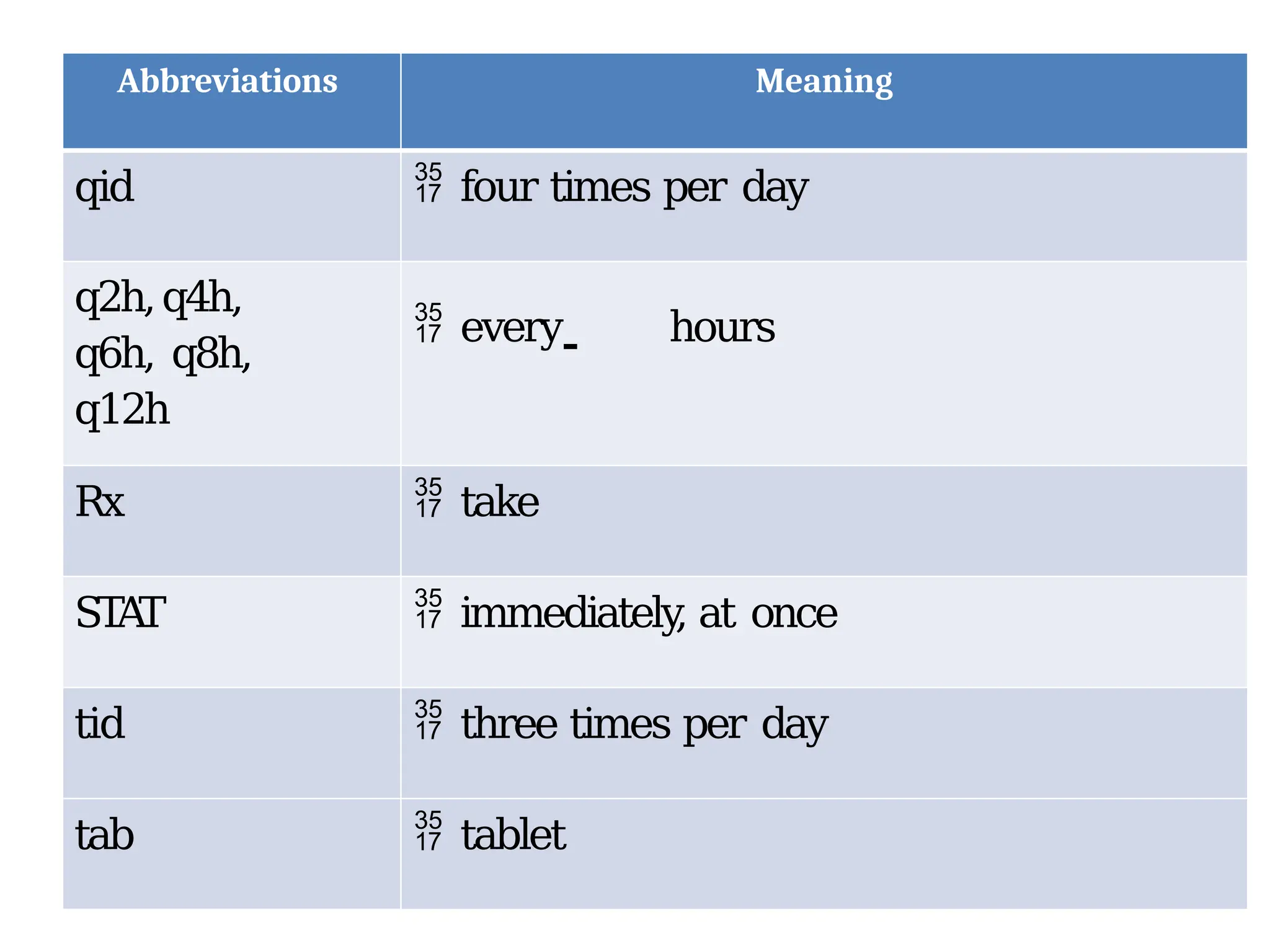
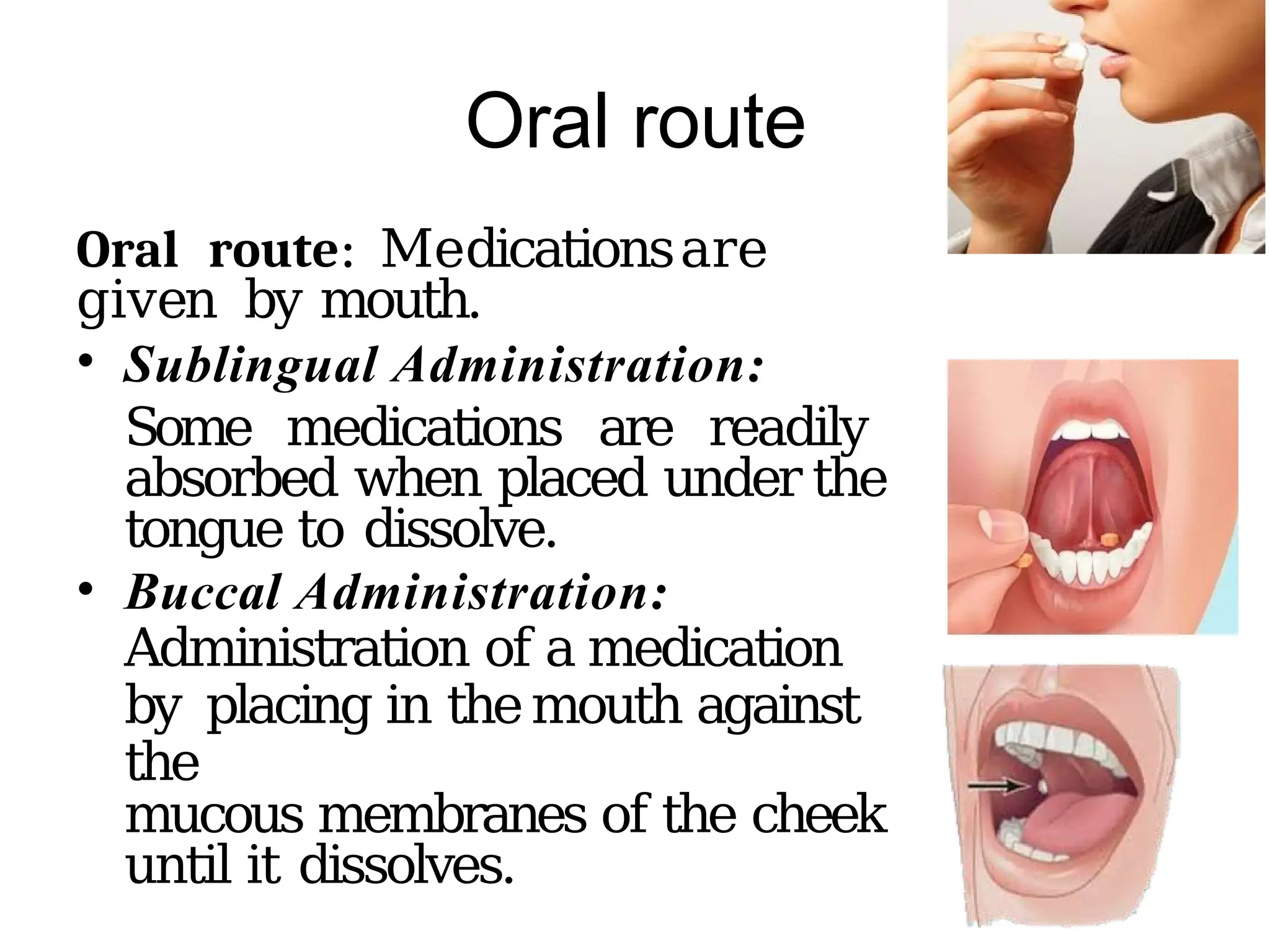
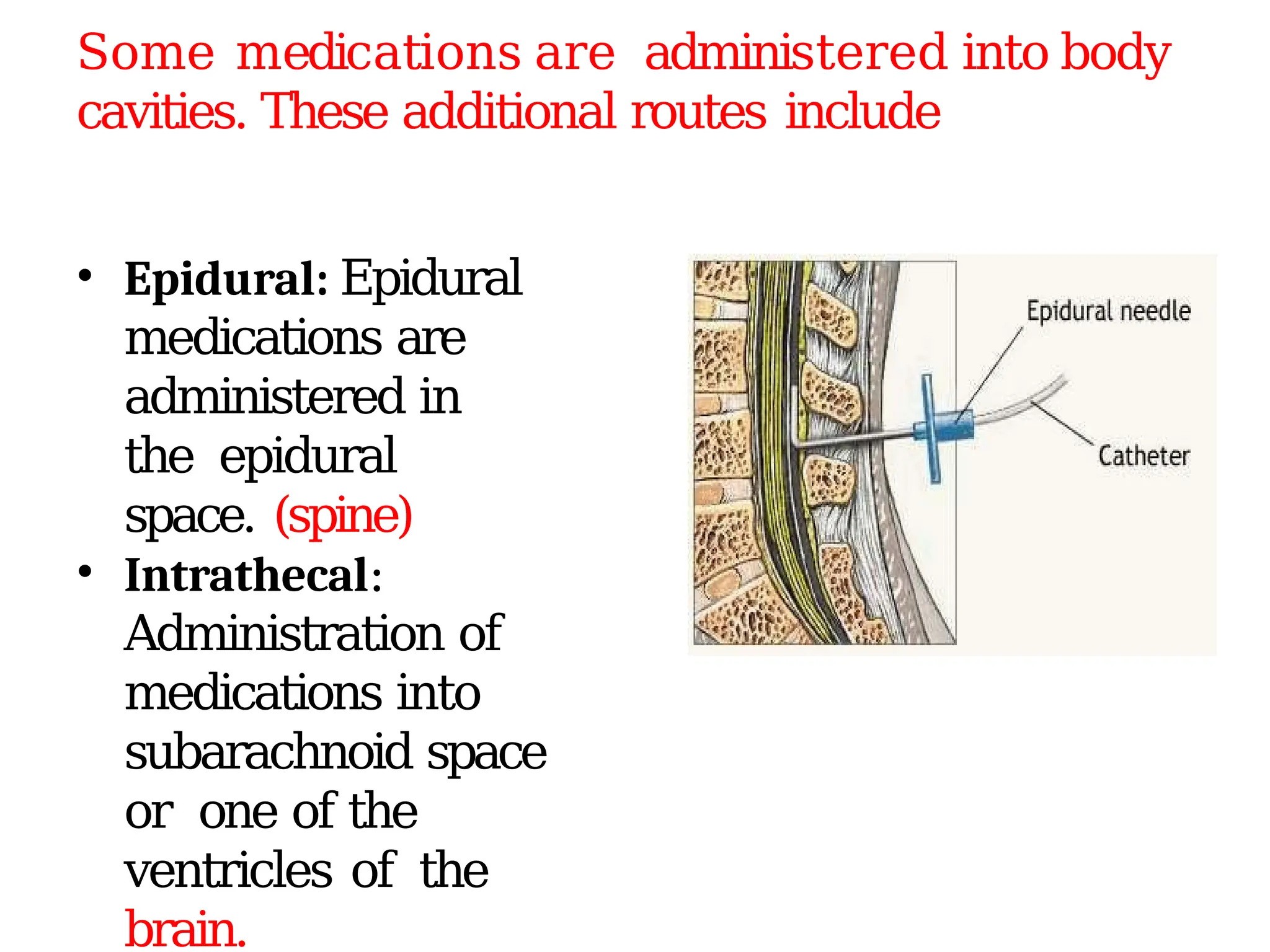
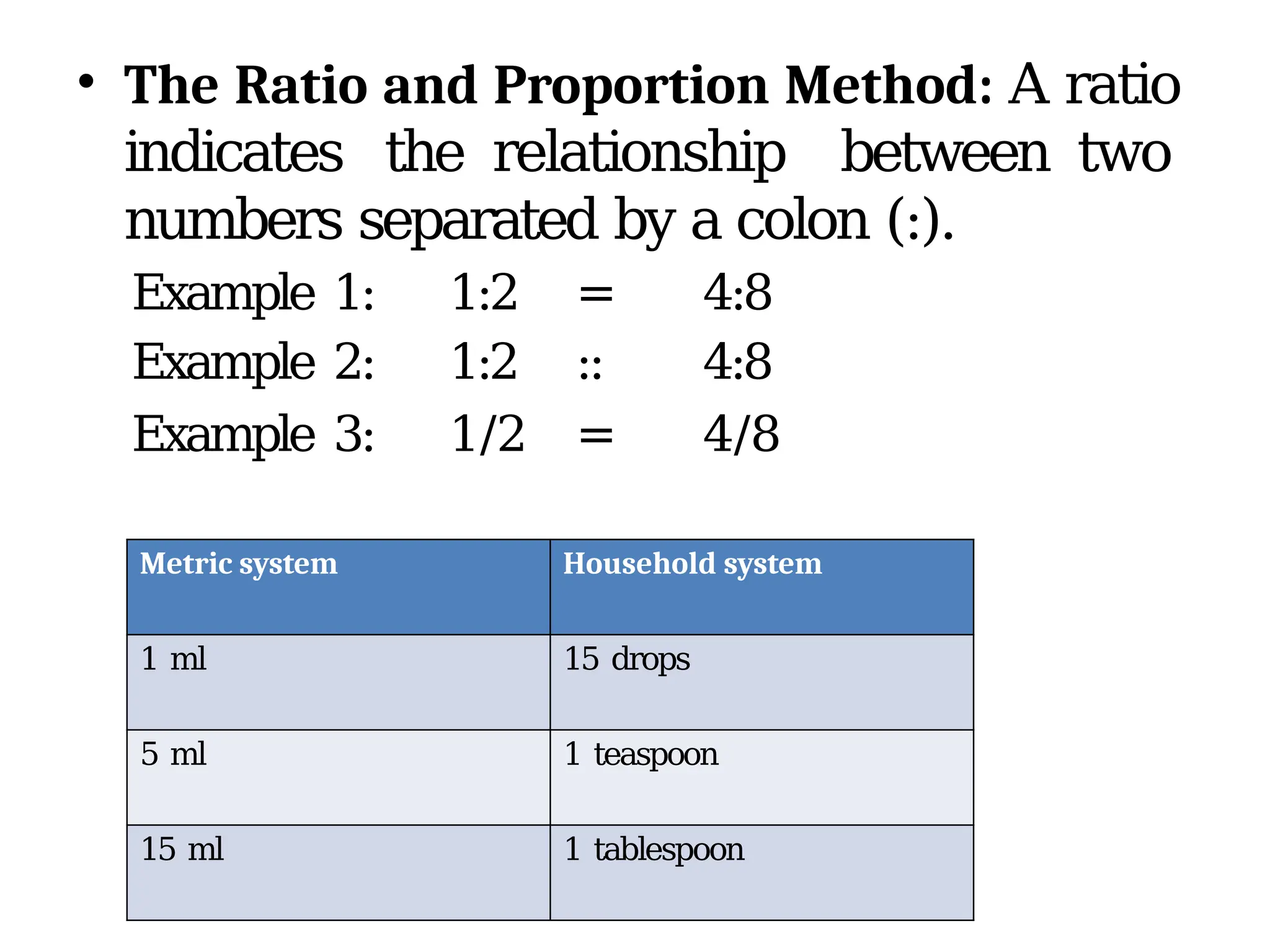
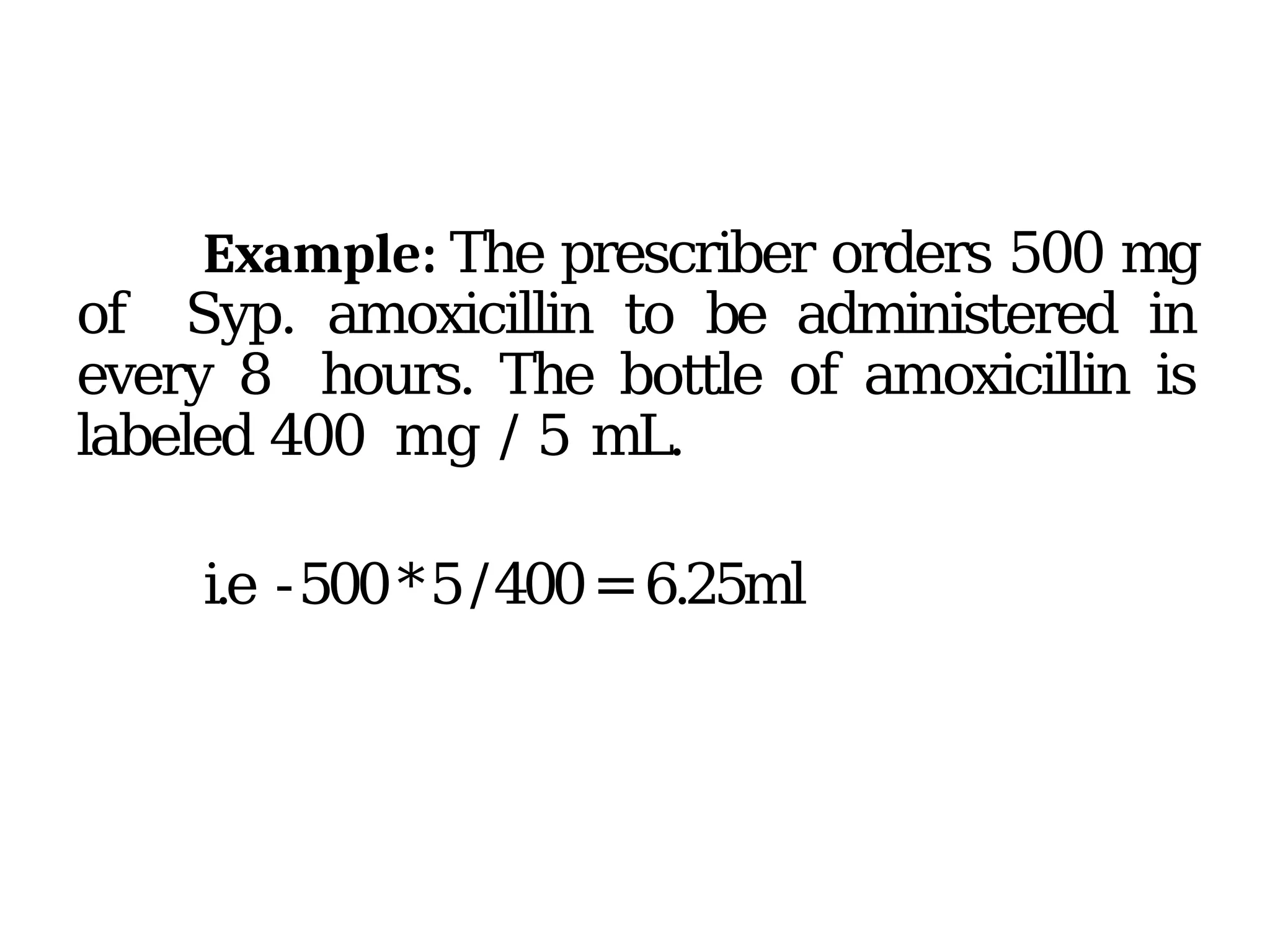
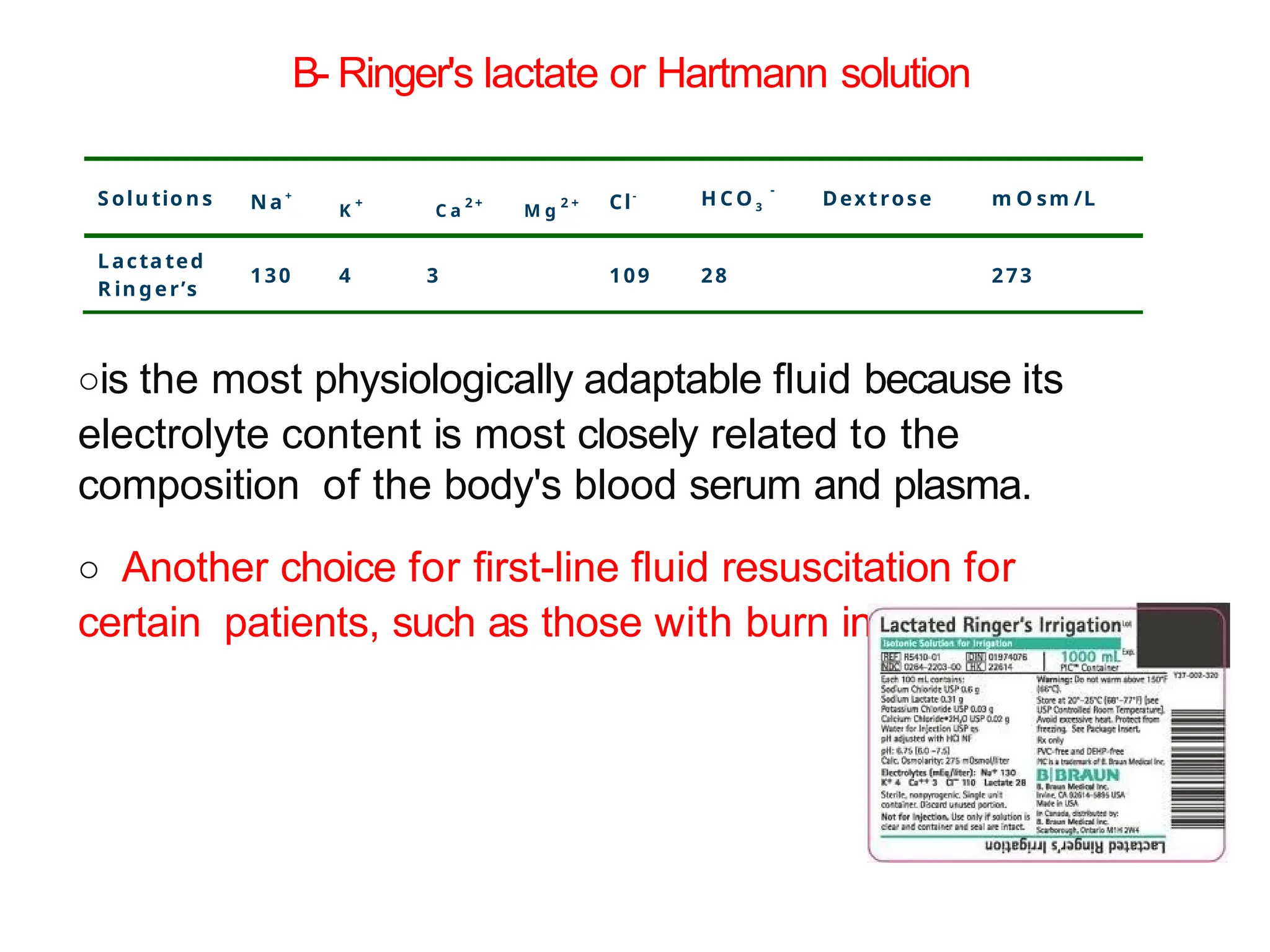
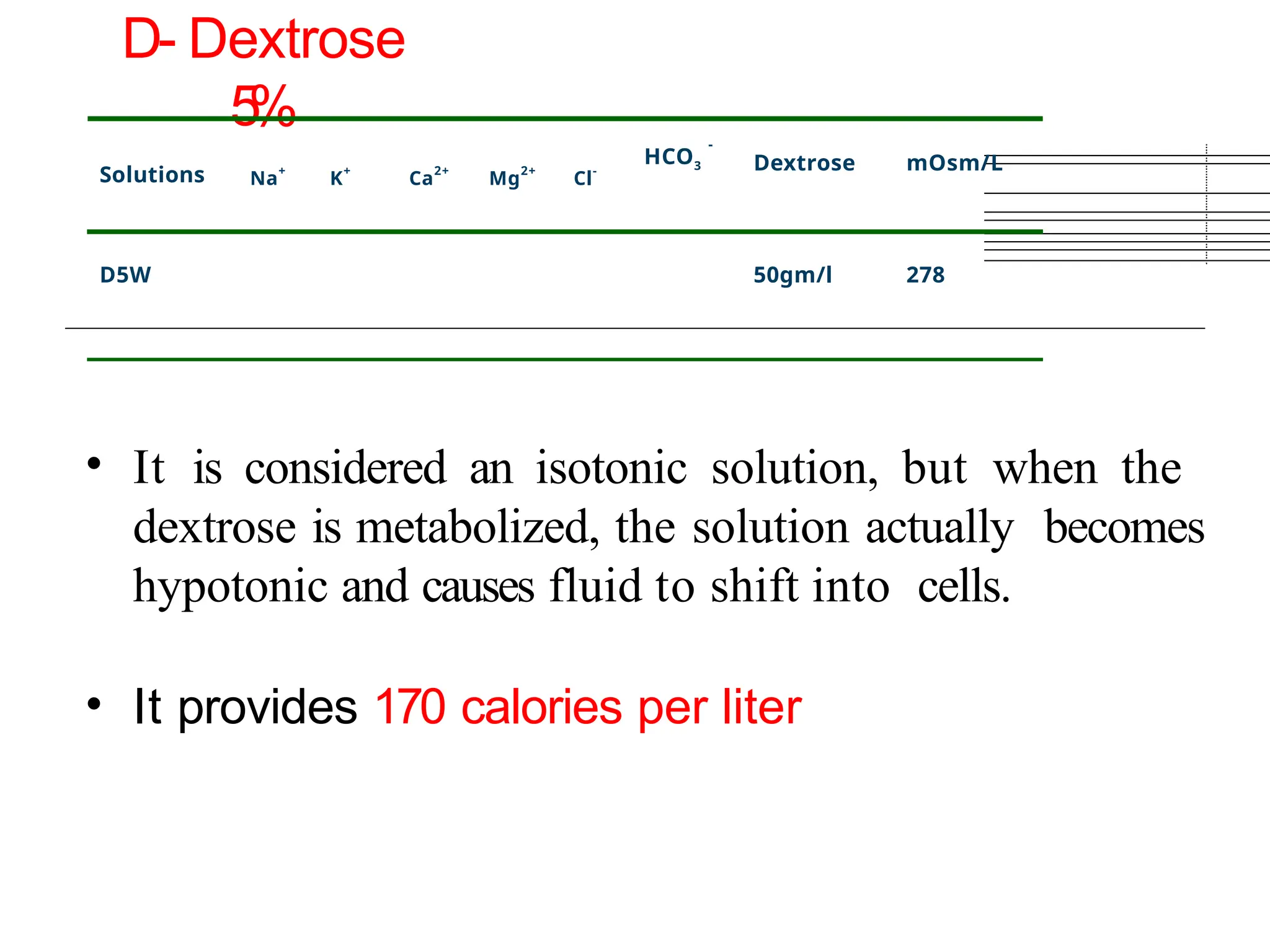
The document outlines various aspects of pharmacology, including medication types, administration principles, storage, and calculations. It explains the significance of medications for prevention, diagnosis, suppression, treatment, and cure, as well as the medication administration rights and checks. Additionally, it provides detailed information on drug forms, routes of administration, and the importance of calculating doses and fluid therapy in clinical practice.