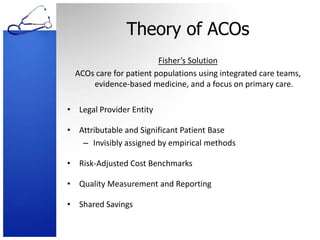
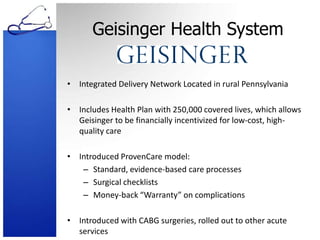
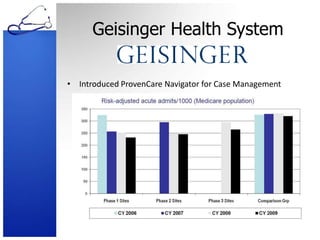
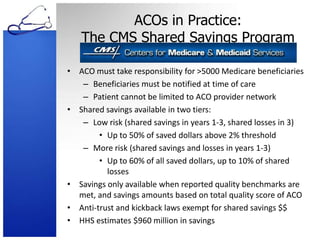
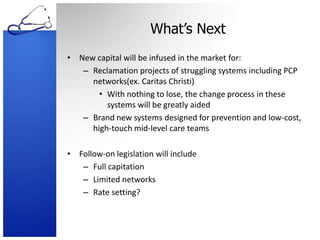
This document discusses Accountable Care Organizations (ACOs) and their design and implementation, as defined by Elliott Fisher in 2009. It highlights the challenges of current healthcare incentives, examples of successful ACO implementations, and the CMS Shared Savings Program established by the Affordable Care Act. The author provides insights on the potential impacts of ACOs on cost and quality of care and anticipates future developments in the healthcare system to support these models.