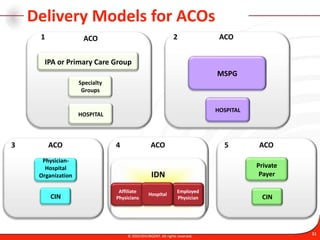
The document provides an overview of accountable care organizations (ACOs) and the role of information technology in ACOs. It describes the goals and program features of Medicare Shared Savings Program ACOs, quality reporting requirements, and necessary health information technology capabilities. It identifies alignment between ACO and meaningful use requirements and presents a potential ACO IT reference model.

















![Quality Reporting MeasuresBetter Care for Individuals Better Health for Populations42 CFR Part 425 [CMS-1345-P]RIN 0938-AQ22 Medicare Program; Medicare Shared Savings Program: Accountable Care Organizations20© 2010 DIVURGENT. All rights reserved.](https://image.slidesharecdn.com/asprez4web061611-110628101555-phpapp01/85/As-prez4web061611-20-320.jpg)























